Understanding sleep deprivation seizures: causes, risks, and what to do
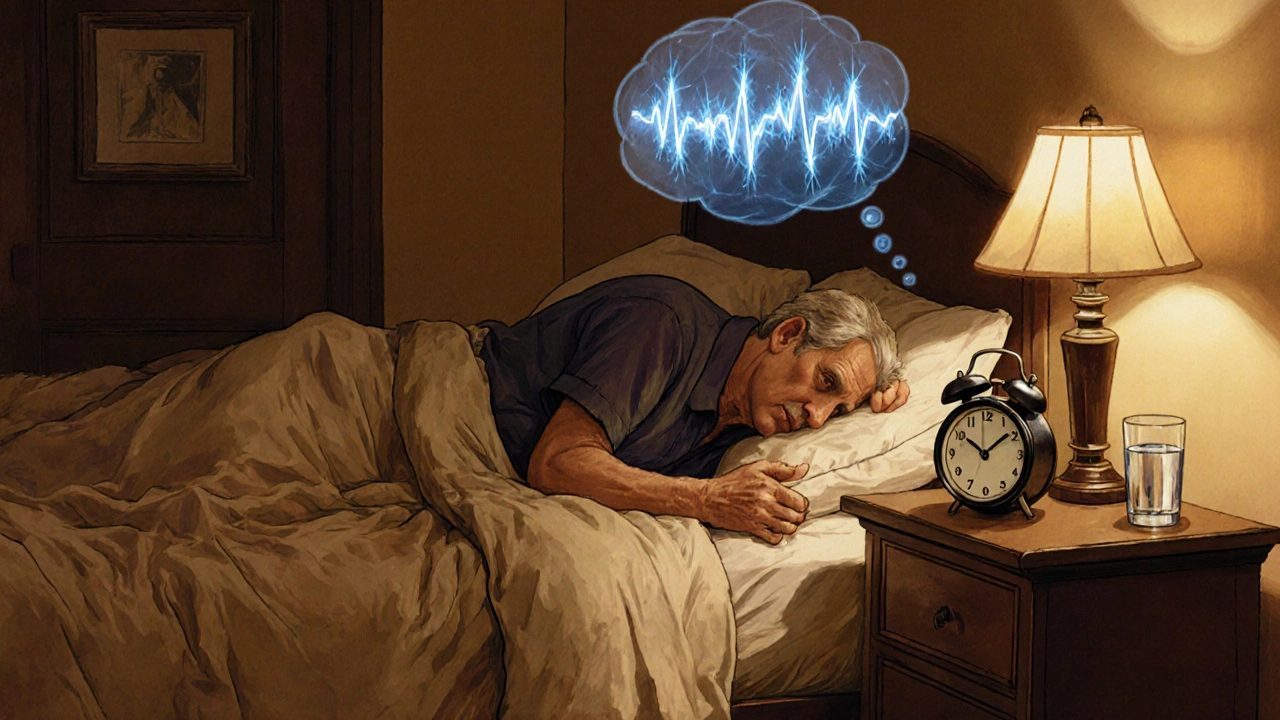
When dealing with sleep deprivation seizures, episodes of convulsive activity triggered by insufficient sleep. Also known as sleep‑related seizures, they often arise in people suffering from sleep deprivation, a state where the body gets less than the recommended 7‑9 hours of rest each night. The underlying seizure occurs when abnormal brain electrical activity crosses a threshold during wake‑sleep cycles, and those with epilepsy are especially vulnerable.
Sleep deprivation itself is more than just feeling tired. It disrupts the balance of neurotransmitters, raises cortisol levels, and reduces the restorative slow‑wave sleep that stabilizes neuronal firing. When you skip a few hours night after night, the brain’s excitability climbs, creating a perfect storm for electrical storms that can manifest as seizures. Even a single night of less than six hours can raise the odds of a seizure event in susceptible individuals.
Seizures are sudden bursts of uncontrolled electrical activity that spread across brain regions. They vary from brief staring spells to full‑body convulsions. While many seizures are unrelated to sleep, the lack of rest removes a natural brake on neuronal hyper‑excitability. In other words, sleep acts like a reset button for brain circuits; without it, the circuits stay primed and can fire off unintentionally.
People with epilepsy already have a lower threshold for seizure onset. Add chronic sleep loss, and that threshold drops further. Studies show that up to 60% of epilepsy patients report more frequent seizures after nights of poor sleep. The link is bidirectional: seizures can also fragment sleep, creating a vicious cycle that’s hard to break without targeted intervention.
At the cellular level, the brain’s glutamate‑GABA balance shifts during sleep deprivation. Glutamate, the main excitatory neurotransmitter, stays elevated, while GABA, the chief inhibitor, drops. This imbalance fuels hyper‑synchronization of neuronal networks, which is a key driver of seizure generation. Imaging studies reveal that sleep‑deprived brains show increased activity in the thalamus and frontal cortex—areas commonly implicated in seizure propagation.
Beyond the basic sleep‑seizure connection, several risk factors amplify the danger. Caffeine overuse, alcohol bingeing, irregular sleep schedules, and high‑stress jobs all heighten brain excitability. Certain medications, like some antidepressants or stimulants, can further lower the seizure threshold when combined with sleep loss. Knowing which personal habits push you toward a seizure can help you make smarter choices.
Diagnosing a sleep deprivation seizure starts with a detailed sleep history and a standard EEG (electroencephalogram) performed after a night of restricted sleep. The EEG captures the brain’s electrical patterns and often reveals spikes or sharp waves that are more pronounced when the patient is sleep‑deprived. In some cases, a 24‑hour video‑EEG monitoring is used to directly correlate sleep loss with seizure events.
Management strategies fall into three buckets: medication adjustment, sleep hygiene, and lifestyle modification. For many, optimizing anti‑seizure drug levels is the first step. Doctors may increase doses or switch to drugs that are less affected by sleep patterns. At the same time, establishing a consistent bedtime, limiting screens before sleep, and creating a dark, quiet bedroom can dramatically cut seizure frequency.
Practical lifestyle tweaks can make a big difference. Aim for the same bedtime and wake‑time every day, even on weekends. Cut caffeine after noon, keep alcohol intake low, and incorporate short, scheduled naps if you’re unable to get a full night’s sleep. Regular exercise helps regulate sleep cycles, but avoid intense workouts right before bedtime. These habits create a stable sleep architecture that keeps the brain’s excitability in check.
Below you’ll find a curated set of articles that dive deeper into each of these areas—from the science behind why lack of sleep sparks convulsions to step‑by‑step guides on improving sleep hygiene, recognizing seizure warning signs, and working with your healthcare team. Whether you’re managing epilepsy, caring for someone who is, or simply curious about the sleep‑seizure link, the resources ahead offer concrete, actionable insights.
Sleep Quality and Seizure Frequency: Understanding the Link
Learn how sleep quality directly impacts seizure frequency, the science behind it, and actionable tips to improve rest for better seizure control.
Read