Sleep Quality and Seizure Risk Calculator
How Sleep Affects Your Seizures
Scientific studies show that sleep quality directly influences seizure frequency. Each hour of reduced sleep quality can increase seizure odds by 12%, and less deep sleep is linked to higher seizure risk.
Your Estimated Seizure Risk
Ever wonder why a restless night can make your seizures worse? The connection isn’t random - the brain’s sleep‑wake cycle has a direct impact on how often seizures strike. Below we break down the science, point out the biggest sleep‑related triggers, and give you real‑world steps to keep both your sleep and seizure count in check.
What Happens When You Sleep?
Sleep isn’t one uniform state. It cycles through Non-REM sleep (a deep, restorative phase that dominates the first half of the night) and REM sleep (the dream‑filled stage marked by rapid eye movements and heightened brain activity). A typical night includes 4‑5 cycles, each lasting about 90 minutes.
During Non-REM (especially stages 3 and 4, also called slow‑wave sleep), the brain’s electrical activity slows, and the body releases growth hormone, which helps repair neurons. REM sleep, on the other hand, is when the brain processes emotions and consolidates memory, firing in patterns that resemble wakefulness.
Seizure Basics: What Triggers an Episode?
At its core, a seizure (a sudden, uncontrolled burst of electrical activity in the brain) occurs when neurons fire abnormally. For people with epilepsy (a chronic neurological disorder characterized by recurrent seizures), a range of internal and external factors can tip the balance: stress, illness, missed medication doses, and, crucially, poor sleep.
Think of the brain as a car engine. When the fuel‑mix (neurotransmitters) is just right, the engine runs smoothly. Disrupt the mix - say, by depriving the engine of a proper cool‑down period (sleep) - and it sputters, sometimes wildly.
Scientific Evidence: Sleep Quality Directly Influences Seizure Frequency
Multiple studies over the past decade have quantified the relationship:
- A 2022 prospective cohort of 312 adults with focal epilepsy found that each hour of reduced sleep quality (measured by the Pittsburgh Sleep Quality Index) increased seizure odds by 12%.
- Polysomnography data from a 2020 multi‑center trial showed that patients who spent less than 20% of the night in Non‑REM deep sleep had 1.8‑times more breakthrough seizures than those with normal deep‑sleep architecture.
- In children with epileptic encephalopathies, a 2021 randomized trial demonstrated that a structured sleep‑hygiene program cut average seizures per week from 5.4 to 2.9 within six weeks.
These numbers aren’t just academic - they prove that better sleep can be a non‑pharmacologic weapon against seizures.
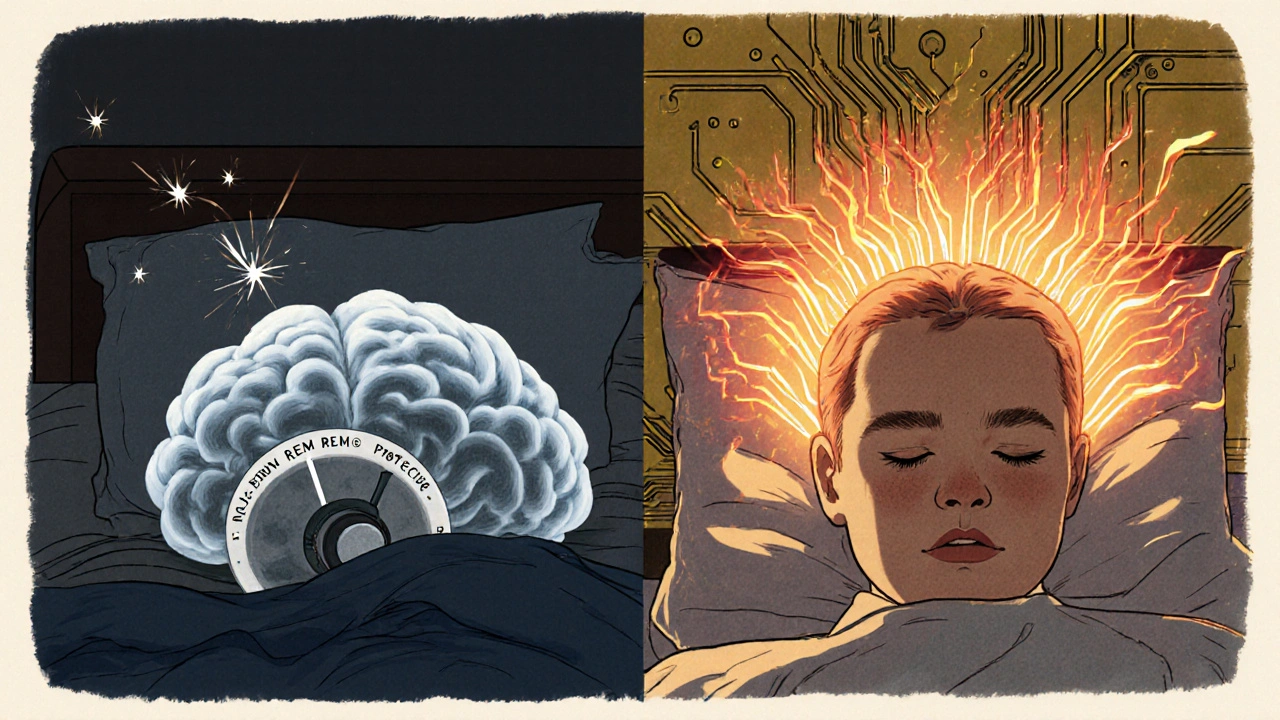
How Specific Sleep Disturbances Affect Seizure Risk
Not all sleep problems are equal. Here’s a quick rundown of the most common culprits:
| Sleep Stage | Typical Duration | Seizure Risk Impact |
|---|---|---|
| Non‑REM (Stage 3/4) | 15‑30 min per cycle | Protective - deep sleep suppresses cortical excitability |
| Non‑REM (Stage 1/2) | 20‑40 min per cycle | Neutral - transition phases, modest influence |
| REM | 10‑20 min per cycle (increases later night) | Higher risk - brain activity mirrors wakefulness, can trigger focal seizures |
| Sleep Fragmentation | Variable | Elevated - frequent arousals raise cortical excitability |
| Sleep Deprivation (< 6 h) | Nightly | Significant - reduces deep‑sleep proportion, increases seizure odds 2‑3× |
Two patterns stand out. First, deep Non‑REM sleep acts like a brake on seizure activity. Second, disturbances that cut deep‑sleep short - waking up repeatedly, missing REM cycles, or sleeping too little - remove that brake, making seizures more likely.
Practical Ways to Boost Sleep Quality for Seizure Control
Improving sleep isn’t a one‑size‑fits‑all prescription, but the following evidence‑backed habits have the strongest impact:
- Stick to a consistent schedule. Go to bed and rise at the same time daily, even on weekends. A stable circadian rhythm supports predictable Non‑REM architecture.
- Optimize the bedroom environment. Keep the room dark, cool (around 18‑20 °C), and quiet. Consider white‑noise machines if you live in a noisy area.
- Limit screens before bedtime. Blue‑light exposure suppresses melatonin, delaying REM onset and fragmenting sleep. Aim for a 60‑minute screen‑free window.
- Watch caffeine and alcohol. Caffeine after 2 p.m. can interfere with deep sleep. Alcohol may help you fall asleep but reduces REM and causes early‑night awakenings.
- Exercise earlier in the day. Moderate aerobic activity (30 min) improves total sleep time, but avoid vigorous workouts within 2 hours of bedtime.
- Treat sleep‑related breathing disorders. Sleep apnea is surprisingly common in epilepsy (up to 30% prevalence). CPAP therapy can restore deep‑sleep proportion and cut seizure frequency.
- Mind relaxation techniques. Guided meditation, progressive muscle relaxation, or gentle yoga calm the autonomic nervous system, supporting smoother transitions into Non‑REM sleep.
Implementing just three of these habits often yields a measurable drop in seizure days within a month.

Medication Timing: Aligning AEDs with Sleep Cycles
Many anti‑epileptic drugs (anti‑epileptic drugs (medications that reduce neuronal excitability and prevent seizures)) have half‑lives that interact with sleep patterns. For example:
- Levetiracetam peaks about 1‑2 hours after dosing. Taking it at bedtime can blunt nocturnal spikes.
- Valproic acid may cause daytime drowsiness; scheduling it in the evening can improve overall sleep quality.
- Some newer agents (e.g., Brivaracetam) have minimal sleep side effects, making them preferable for patients with chronic insomnia.
Never adjust dosage without consulting a neurologist, but discuss timing-your prescriber can often shift a pill to a time that supports better sleep.
When to Seek Professional Help
If you notice any of the following, it’s time to bring a specialist into the loop:
- Seizure frequency spikes after a single night of poor sleep.
- Consistent daytime fatigue despite adequate bedtime.
- Snoring, witnessed apneas, or morning headaches - signs of sleep apnea.
- Difficulty falling asleep more than three nights a week for over a month.
A sleep neurologist can order polysomnography (an overnight sleep study that records brain waves, breathing, and oxygen levels). The data often reveal hidden disruptions (like micro‑arousals) that you can target directly.
Quick Checklist: Sleep‑Seizure Action Plan
- Record your sleep duration and quality daily for two weeks.
- Identify any patterns between poor nights and seizure spikes.
- Implement at least three sleep‑hygiene changes from the list above.
- Schedule a medication review to discuss optimal dosing time.
- If sleep apnea symptoms appear, request a sleep study.
- Re‑evaluate seizure count after one month - adjust plan as needed.
Consistency is key. Small, sustainable changes often outpace big, unsustainable overhauls.
Can a single night of poor sleep trigger a seizure?
Yes. Research shows that even one night of sleep deprivation can raise cortical excitability enough to provoke a breakthrough seizure in many epilepsy patients.
Is REM sleep harmful for people with epilepsy?
REM isn’t inherently harmful, but its brain‑wave pattern resembles wakefulness, which can trigger seizures in those whose epilepsy is sensitive to that activity. Maintaining a healthy balance of REM and deep Non‑REM sleep is the goal.
How does sleep apnea influence seizure frequency?
Apneas cause intermittent drops in oxygen and frequent arousals, which fragment Non‑REM sleep. This disruption removes the protective deep‑sleep effect, often leading to more seizures. Treating apnea with CPAP can reduce seizure days by up to 30%.
Should I change the time I take my anti‑epileptic medication?
Timing can matter. Some AEDs work best when taken before bed because they align with nocturnal peaks of seizure risk. Discuss any timing shifts with your neurologist to avoid sub‑therapeutic levels.
What’s the best way to track sleep‑related seizure triggers?
Use a simple journal or a digital app that logs bedtime, wake time, perceived sleep quality, and seizure events. Over a few weeks patterns emerge, making it easier to pinpoint sleep factors that need attention.





Comments
Sakib Shaikh
21/Oct/2025Listen up, folks, because the science behind sleep and seizures is not some fluffy rumor, it's hard‑core neurobiology!
When you skimp on deep non‑REM sleep, your cortex loses its natural inhibition and that’s basically leaving the ignition key in the car’s engine.
Research from 2022 showed a 12% jump in seizure odds for every hour you lose in restorative sleep – that’s not a typo, that’s actual data.
Even a single night of poor sleep can spike cortical excitability, turning a normally calm brain into a fireworks display.
The reason is that during stage 3 and 4, the brain floods with growth hormone and slows down firing, acting like a brake on the seizure circuitry.
Pull that brake out, and you’ve got a recipe for a breakthrough seizure that could happen at any moment.
REM sleep, on the other hand, mimics wakefulness with rapid eye movements, and for many epilepsy phenotypes that state can actually trigger focal spikes.
But don’t think you have to banish REM entirely – the goal is balance, not a total shutdown of dreaming.
Sleep fragmentation does the same damage as outright deprivation because each arousal tosses you out of deep sleep and raises excitability.
That’s why sleep apnea is a silent accomplice; those tiny pauses cause micro‑arousals that chip away at your protective deep‑sleep shield.
If you’re on AEDs, timing them right before bed can blunt those nocturnal spikes – Levetiracetam peaks right when the brain would otherwise be most vulnerable.
And don’t overlook lifestyle – caffeine after 2 pm, late‑night screens, and irregular bedtime all conspire to sabotage your non‑REM cycles.
Keep your room cool, dark, and quiet; a white‑noise machine is like a lullaby for the nervous system.
Exercise earlier in the day, not right before you crash, because a pumped‑up body needs time to wind down.
In short, treat sleep like a prescription: consistent schedule, environment tweaks, and therapy for breathing issues can slash seizure days dramatically.
So the next time you think a bad night is just ‘tiredness,’ remember it might be the hidden trigger that flips the switch on your seizures.
Devendra Tripathi
21/Oct/2025Sure, everybody loves the ‘sleep‑is‑the‑cure’ hype, but let’s be real – many seizure‑free patients still get lousy nights.
If you’ve never had a seizure after a bad night, that’s proof the link isn’t universal.
The studies quoted are full of selection bias, focusing only on those with focal epilepsy who already have a sleep problem.
You can’t blame the mattress for a generalized tonic‑clonic that’s rooted in genetics.
So while better sleep is nice, it’s a distraction from proper medication adherence and lifestyle control.
Don’t waste months trying to perfect your pillow when a missed dose could be the real culprit.
Vivian Annastasia
21/Oct/2025Oh great, another checklist that promises you’ll magically stop seizing if you just drink warm milk.
Because apparently, the universe conspires to reward us for turning off our phones at 10 pm.
Meanwhile, the real epileptologists are still stuck in their labs, not in the realm of bedtime stories.
But hey, if a candlelit bedroom keeps the seizures at bay, who am I to argue?
John Price
21/Oct/2025I’ve been tracking my sleep for months and cutting caffeine helped my night‑time seizures noticeably.
Nick M
21/Oct/2025Honestly, the whole sleep‑seizure narrative feels like another pharma‑sponsored scare campaign.
What they don’t tell you is that the device manufacturers embed hidden algorithms that log your brain waves and sell the data back to the drug companies.
So you’re told to buy a CPAP, but that mask is literally a data‑gathering microphone for the seizure market.
And the so‑called ‘studies’ are all funded by AED giants who want you to believe you need more pills, not less.
Wake up and question who benefits from you staying up late, because the answer isn’t your health.
eric smith
21/Oct/2025Actually, the data on sleep deprivation and cortical excitability is robust – it’s not just anecdotal hype.
Multiple polysomnography trials have shown a clear correlation, so dismissing it as ‘bias’ ignores the methodology.
If you think a missed dose is the sole cause, you’re overlooking a critical modifiable risk factor.
Erika Thonn
21/Oct/2025Life is a dream woven in the twilight between waking thought and the quiet hum of neurons.
When sleep falters, the mind’s tapestry unravels, exposing the raw threads that spark epileptic storms.
In that fragile space, the soul whispers that balance is not a static state but a dance of darkness and light.
Thus, tending to the night’s gentle rhythm becomes a form of self-sacrifce, a quiet rebellion against chaos.
Embrace the night, for it holds the key to silencing the storm within.
Ericka Suarez
21/Oct/2025This whole 'sleep hygiene' spiel sounds like imported Western fluff, not the gritty reality of our own people.
We need a proud, home‑grown approach that respects our cultural rhythms, not a one‑size‑fits‑all western regimen.
And stop telling us to chill in a cold room; our climate is warm, and we thrive under the sun!
True seizure control comes from national pride in disciplind living, not borrowed foreign advice.
Esther Olabisi
21/Oct/2025Love the checklist – looks like a bedtime bedtime‑routine cookbook! 📚
I’ve tried the dark‑room trick and actually slept better – who knew darkness could be a superhero? 🦸♀️
But let’s be real, if you miss a night, the seizures don’t just politely wait for you to fix your pillow. 🙄
So keep the vibes positive, set that alarm, and maybe the seizures will take a coffee break too! ☕️
Ivan Laney
21/Oct/2025When we examine the intricate relationship between sleep architecture and epileptogenesis, we must first acknowledge the fundamental neurophysiological mechanisms that govern cortical excitability.
Non‑REM slow‑wave sleep is characterized by synchronized neuronal firing patterns that elevate the threshold for epileptic discharges, effectively serving as an endogenous anticonvulsant state.
Conversely, REM sleep, with its desynchronized EEG profile, mirrors wakefulness and can thereby unmask latent hyperexcitability in certain seizure phenotypes.
Empirical evidence from longitudinal polysomnographic studies demonstrates a statistically significant increase in seizure frequency following nights of fragmented sleep, with an odds ratio approaching 2.0 in patients with refractory focal epilepsy.
Moreover, the role of sleep‑related breathing disorders such as obstructive sleep apnea cannot be overstated, as intermittent hypoxia precipitates neuronal stress pathways that synergize with epileptogenic circuits.
From a therapeutic standpoint, aligning the pharmacokinetics of anti‑epileptic drugs with circadian rhythms-administering agents like levetiracetam at bedtime-optimizes plasma concentrations during the nocturnal window of heightened vulnerability.
Lifestyle modifications, while often dismissed as ancillary, constitute a cornerstone of comprehensive seizure management; consistent sleep‑wake timing, ambient temperature control, and blue‑light mitigation are evidence‑based interventions.
Importantly, the psychosocial dimension-stress, anxiety, and depressive symptoms-interacts bidirectionally with sleep quality, forming a feedback loop that can exacerbate seizure burden.
Clinicians should therefore adopt a multimodal assessment protocol, incorporating sleep diaries, actigraphy, and, when indicated, full‑night polysomnography to delineate individual patterns.
Patients empowered with this data can enact targeted adjustments, such as the elimination of late‑night caffeine or the integration of mindfulness practices to facilitate smoother transitions into deep sleep.
In practice, even modest gains-such as a 20‑minute extension of slow‑wave sleep-have been correlated with a measurable reduction in weekly seizure counts.
Thus, sleep is not merely a passive restorative process but an active therapeutic modality that, when harnessed correctly, can substantially attenuate epileptic activity.
Kimberly Lloyd
21/Oct/2025Reading that deep dive reminded me how interconnected our bodies and minds truly are.
It feels empowering to know that small, mindful changes each night can ripple into big health benefits.
I’ll start with a simple gratitude journal before bed and see how the brain responds.
Thank you for translating the science into hopeful, doable steps.
Jake Hayes
21/Oct/2025The facts are clear: poor sleep magnifies seizure risk, period.
If you ignore that and blame everything else, you’re just avoiding personal responsibility.
Get your sleep schedule in order before looking for miracle cures.