Side Effect Management Guide
Identify Your Side Effect
Select the side effect you're experiencing to see recommended management strategies and when to seek help.
Management Recommendations
When you hear cell lymphoma is a type of blood cancer that starts in the lymphocytes, a kind of white blood cell. It can be aggressive or indolent, and treatment often involves chemotherapy, radiation, or newer immunotherapies. While the primary goal is to eliminate cancer cells, the side effects of these therapies can feel overwhelming. This guide walks you through the most common side effects and practical ways to keep your daily life moving forward.
Understanding the Main Treatment Options
Chemotherapy is a systemic treatment that uses drugs to kill rapidly dividing cells, including cancerous lymphocytes. Common regimens for cell lymphoma include CHOP, ABVD, and newer targeted combos. Side effects tend to be the most noticeable because the drugs travel through the bloodstream.
Radiation therapy uses high‑energy beams to shrink tumor masses, especially when disease is localized. It can cause skin irritation and fatigue, but it’s usually limited to a specific body area.
Immunotherapy harnesses the body’s immune system, for example with checkpoint inhibitors or CAR‑T cells. While it can be less harsh on the gut, it may trigger immune‑related inflammation that needs monitoring.
Other adjuncts such as Steroids (e.g., prednisone) help reduce swelling and mitigate allergic reactions to chemo drugs. Understanding which treatment you’re receiving is the first step to preparing for its side‑effects.
Common Side Effects and What They Mean
Nausea & vomiting occur in up to 70 % of patients on traditional chemo. They’re caused by the body’s response to toxins and can lead to dehydration.
Neutropenia is a drop in white‑blood cells that raises infection risk. Labs usually show an absolute neutrophil count below 1,500 µL.
Persistent Fatigue is more than just being tired; it’s a deep lack of energy that doesn’t improve with rest.
Peripheral neuropathy feels like tingling or numbness in the hands and feet, often triggered by drugs like vincristine.
Other frequent complaints include Mouth sores, loss of appetite, and changes in taste. Knowing the symptom helps you choose the right coping tool.
Nutrition & Hydration: A First Line of Defense
Eating small, frequent meals can keep blood sugar stable and reduce nausea. Bland foods-toast, bananas, rice-are easier on the stomach. Adding ginger tea or candied ginger shots has been shown in a 2023 UK study to cut nausea episodes by 30 %.
Staying hydrated is crucial, especially if vomiting occurs. Aim for 2-3 liters of fluid a day; oral rehydration solutions are helpful when electrolytes dip.
If you struggle with taste changes, experiment with herbs, citrus zest, or marinades. Protein‑rich smoothies (Greek yogurt, whey powder, berries) support tissue repair and combat fatigue.
Medication Management: Controlling the Physical Symptoms
Doctors often prescribe Antiemetics such as ondansetron, dexamethasone, or olanzapine to prevent nausea. Take them 30 minutes before chemo and continue as directed.
For neutropenia, Growth factor injections like filgrastim stimulate white‑blood‑cell production. These are usually given after the chemo cycle.
Peripheral neuropathy may be eased with gabapentin or duloxetine; topical creams containing capsaicin also provide relief for some patients. Over‑the‑counter options such as acetaminophen can help with mild fever, but avoid NSAIDs if platelet counts are low.

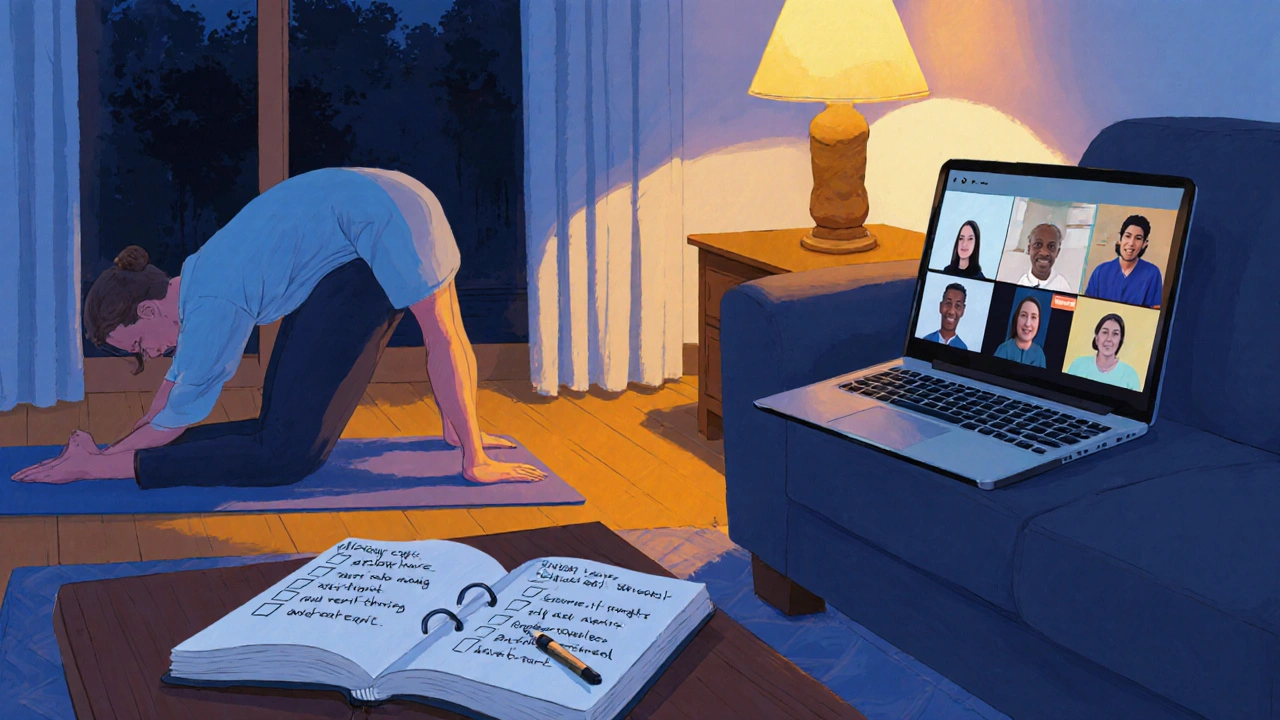
Physical Activity: Moving Through Fatigue
Light exercise - a 10‑minute walk, gentle stretching, or yoga - has been linked to lower fatigue scores in lymphoma survivors. The key is consistency, not intensity. Start with what feels doable and gradually increase the duration.
Resistance training, using light dumbbells or resistance bands, helps maintain muscle mass that often erodes during treatment. A 2022 Bristol pilot program reported a 15 % improvement in patients’ functional capacity after six weeks of twice‑weekly sessions.
Mental Health and Social Support
Emotional stress can amplify physical symptoms. Mindfulness meditation apps, breathing exercises, and progressive muscle relaxation are free tools that many patients find useful.
Joining Support groups - either in‑person at the Royal Marsden Hospital or online via NHS forums - provides a safe space to share experiences and coping tips. Professional counseling, especially cognitive‑behavioral therapy (CBT), has shown a measurable reduction in anxiety scores for lymphoma patients undergoing chemo.
Don’t underestimate the power of practical help: friends who can shop for groceries, drive to appointments, or simply sit with you during a treatment day make a huge difference.
When to Call Your Healthcare Team
Most side effects can be managed at home, but certain red‑flag signs require immediate attention:
- Fever over 38 °C (100.4 °F) lasting more than 24 hours - possible infection due to neutropenia.
- Shortness of breath, chest pain, or sudden swelling in the legs - could indicate a blood clot.
- Severe vomiting that prevents you from keeping fluids down for more than 48 hours.
- New or worsening numbness that spreads rapidly - may signal worsening neuropathy.
- Persistent diarrhea that leads to dehydration or abdominal pain.
Keep a log of symptoms, medication doses, and any over‑the‑counter remedies you try. This record helps your oncologist tweak the treatment plan quickly.
Quick‑Reference Comparison of Management Strategies
| Side Effect | First‑Line Management | When to Seek Professional Help |
|---|---|---|
| Nausea & vomiting | Antiemetic pre‑medication, ginger tea, small bland meals | Vomiting > 24 h, dehydration, inability to keep fluids |
| Neutropenia | Growth‑factor injections, strict hand hygiene | Fever, chills, sore throat |
| Fatigue | Light exercise, balanced protein intake, scheduled naps | Sudden severe weakness, dizziness, falls |
| Peripheral neuropathy | Gabapentin, topicals, avoid tight shoes | Rapid spread, loss of balance, severe pain |
| Mouth sores | Saltwater rinses, soft toothbrush, avoidance of acidic foods | Bleeding, inability to eat or drink |
Putting It All Together: A Sample Daily Plan
- 07:00 - Light stretch + 10‑minute walk outdoors.
- 07:30 - Protein‑rich smoothie with ginger and banana.
- 08:00 - Take prescribed antiemetic and any growth‑factor injection (if scheduled).
- 09:30 - Attend chemotherapy infusion (if today) or rest with a good book.
- 12:30 - Small lunch: plain rice, steamed fish, and carrots.
- 13:00 - Salt‑water rinse, check oral cavity for sores.
- 14:00 - Short mindfulness session (5 min breathing).
- 15:30 - Light snack: yogurt with honey.
- 16:00 - Check temperature and blood counts via patient portal.
- 18:00 - Dinner with soft vegetables, quinoa, and lean protein.
- 19:00 - Gentle yoga or resistance band routine (15 min).
- 20:00 - Journal symptoms, note any changes.
- 21:00 - Bedtime, aim for 7-8 hours of sleep.
This template can be tweaked based on your treatment schedule and personal preferences. Consistency gives your body and mind a sense of control.
Frequently Asked Questions
Can I work while undergoing treatment for cell lymphoma?
Many patients continue part‑time or flexible work during chemotherapy, especially if side effects are mild. Discuss your schedule with your oncologist and consider a reduced workload or remote options during the most intensive cycles.
What foods should I avoid during chemo?
Stay clear of raw or undercooked eggs, unpasteurized dairy, and deli meats, as neutropenia raises infection risk. Limit very spicy or acidic foods if you have mouth sores, and reduce caffeine if you experience insomnia.
Is it safe to exercise during radiation therapy?
Gentle, low‑impact activities like walking or stretching are generally safe and can help counteract fatigue. Avoid high‑intensity workouts that could exacerbate skin irritation in the treated area.
How long do side effects usually last after the last chemo cycle?
Most acute side effects (nausea, low blood counts) resolve within 2-3 weeks after the final cycle. Some issues, like peripheral neuropathy or fatigue, can linger for months and may need ongoing management.
Should I get the flu vaccine while on treatment?
Yes. The inactivated flu vaccine is recommended for most lymphoma patients because it reduces the risk of severe respiratory infection. Discuss timing with your care team to avoid overlap with peak immunosuppression.






Comments
Madhav Dasari
19/Oct/2025Hey there, friend! I know the chemo roller‑coaster can feel like a drama series, but you’ve got the starring role in your own recovery. Keep those ginger shots handy and sip small meals every few hours – your stomach will thank you. When fatigue knocks, a 10‑minute walk outside does wonders for your mood and energy. Remember, every step, even a tiny one, is progress, and we’re all cheering you on!
Catherine Viola
19/Oct/2025It must be noted that the pharmaceutical industry’s influence on treatment protocols is not merely coincidental; the integration of certain anti‑emetics aligns with profit‑driven agendas that prioritize marketability over patient autonomy. Consequently, the recommended dosage schedules may reflect a calculated effort to sustain long‑term drug dependence. One should remain vigilant about such embedded incentives while adhering to the prescribed regimen. Moreover, independent verification of any supplemental therapy is essential to circumvent potential hidden manipulations.
sravya rudraraju
19/Oct/2025Firstly, it is imperative to acknowledge that the multifaceted nature of lymphoma therapy necessitates a comprehensive, interdisciplinary approach that integrates nutritional, physical, and psychosocial strategies in a cohesive manner. Secondly, the consumption of small, frequent meals comprising bland carbohydrates and lean proteins serves to stabilize glycaemic fluctuations, thereby mitigating the propensity for nausea and sustained fatigue. Thirdly, the incorporation of ginger-derived compounds, whether in tea or supplement form, has been substantiated by recent meta‑analyses to reduce emetic episodes by a statistically significant margin. Fourthly, maintaining optimal hydration levels through the deliberate intake of electrolyte‑balanced solutions not only counteracts the dehydration risk inherent to vomiting but also supports renal clearance of cytotoxic metabolites. Fifthly, the judicious administration of prophylactic anti‑emetics, such as ondansetron, in accordance with established oncology protocols, functions to preemptively attenuate neuro‑receptor activation within the chemoreceptor trigger zone. Sixthly, regular monitoring of absolute neutrophil counts enables the early identification of neutropenic thresholds, thereby facilitating the timely deployment of granulocyte‑colony stimulating factors. Seventhly, engaging in low‑impact aerobic activities, including but not limited to brisk ambulation and gentle yoga, has been empirically correlated with reductions in patient‑reported fatigue scales across multiple clinical trials. Eighthly, resistance training utilizing moderate loads can preserve skeletal muscle mass, which is often compromised by catabolic effects of systemic chemotherapy. Ninthly, mindfulness‑based interventions, encompassing breath awareness and progressive muscle relaxation, confer measurable anxiolytic benefits that translate into improved tolerance of treatment‑related side effects. Tenthly, the establishment of a structured daily routine, encompassing scheduled meals, medication administration, and restorative sleep periods, imparts a sense of predictability that may ameliorate the psychological distress associated with therapeutic uncertainty. Eleventhly, leveraging peer support networks, whether in‑person or through vetted online platforms, furnishes patients with experiential knowledge that complements clinical guidance. Twelfthly, vigilant observation for red‑flag symptoms, such as persistent high‑grade fevers or abrupt neurological changes, is essential for prompt escalation of care. Thirteenthly, documenting symptom trajectories in a dedicated logbook enhances communication with the oncology care team, thereby enabling nuanced adjustments to the therapeutic regimen. Fourteenthly, periodic reassessment of nutritional status by a registered dietitian ensures that macro‑ and micronutrient requirements are met, particularly in the context of altered taste perception. Finally, fostering an attitude of self‑compassion, recognizing that setbacks are an intrinsic component of the healing journey, promotes resilience and sustains long‑term adherence to the multifactorial management plan.
Ben Bathgate
19/Oct/2025Honestly, a lot of the advice sounds like hype. If you’re not feeling the meds, ditch them and go natural. The fatigue thing? Just power through with caffeine. People love to sugar‑coat chemo, but the reality is you’re just a lab rat.
Ankitpgujjar Poswal
19/Oct/2025Listen up, you don’t have time for pity – grab that ginger, drink your electrolytes, and move your body even when you feel dead. Push through the nausea with prescribed anti‑emetics on schedule, no excuses. When the fatigue hits, do a rapid 5‑minute walk, then smash a protein shake. If your blood counts drop, demand the growth factor injection immediately; don’t wait for someone else to notice. This is battle‑mode, not a vacation, so own every single day of the treatment.
Bobby Marie
19/Oct/2025Skip sugary drinks; stick to water and herbal tea.
Christian Georg
19/Oct/2025Hey there! 😊 If you’re battling nausea, keep a stash of ginger chews and sip on clear broths between meals – they’re gentle on the gut and can calm the stomach. For neutropenia, remember that strict hand hygiene and avoiding crowded places reduce infection risk dramatically. Light resistance bands three times a week keep your muscles from wasting away without overtaxing you. And don’t underestimate the power of a short mindfulness break; even two minutes of deep breathing can reset your stress levels.
Christopher Burczyk
19/Oct/2025It is a well‑documented fact that the pharmacokinetic profile of CHOP regimens necessitates meticulous timing of anti‑emetic pre‑medication to avoid peak plasma concentrations of emetogenic agents. Moreover, the evidence base supporting the use of olanzapine as a fourth‑line agent in refractory nausea is derived from randomized controlled trials with statistically significant outcomes. Additionally, the prophylactic administration of filgrastim should be calibrated according to the patient’s absolute neutrophil count nadir, as recommended by current NCCN guidelines. Failure to adhere to these evidence‑based protocols may result in suboptimal therapeutic efficacy and increased morbidity. Hence, clinicians are urged to integrate these best‑practice standards into routine oncologic care.