After surgery, pain is inevitable-but how you manage it can make all the difference. For years, the default answer was opioids: morphine, oxycodone, hydromorphone. But that approach came with serious risks-addiction, nausea, constipation, even respiratory depression. Today, a smarter, safer method is taking over: multimodal analgesia (MMA). It’s not a single drug. It’s a strategy. And it’s now the standard of care for most surgeries.
What Is Multimodal Analgesia?
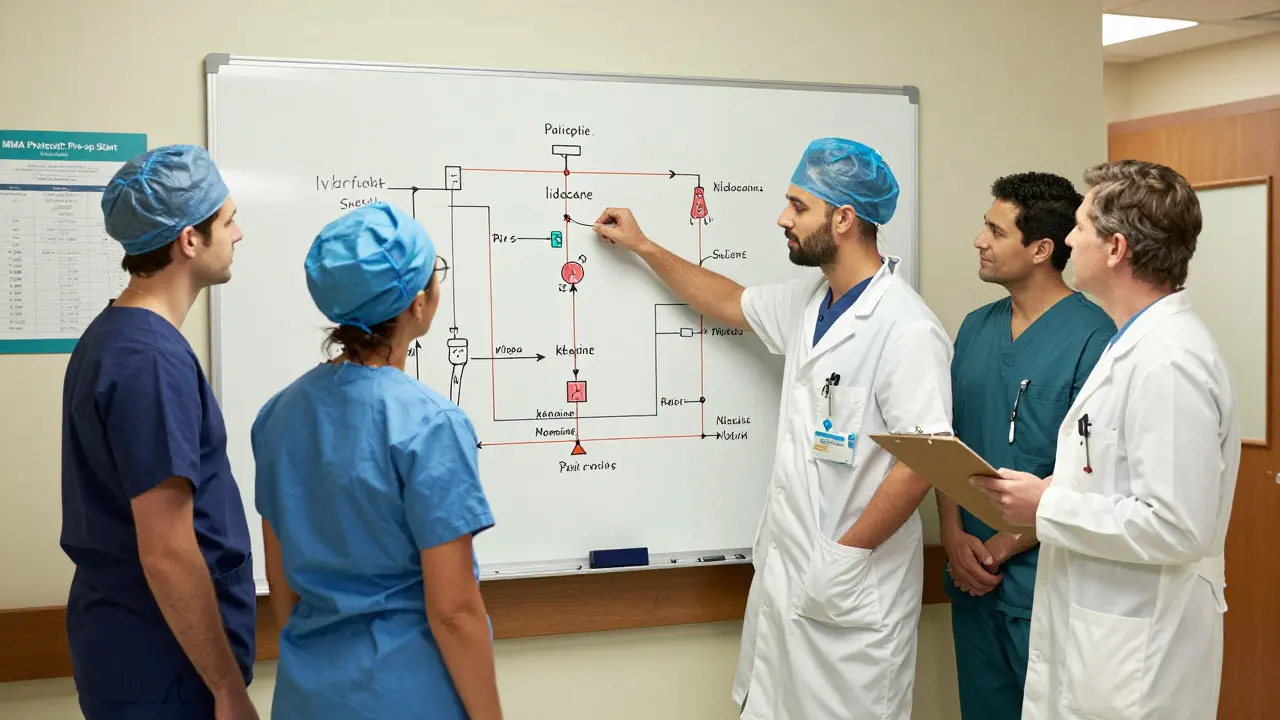
Multimodal analgesia means using more than one type of pain reliever at the same time, each targeting a different part of the pain pathway. Think of it like blocking pain at multiple checkpoints instead of relying on one roadblock. This approach lets doctors use lower doses of each medication, which means fewer side effects. The goal isn’t to eliminate opioids completely-it’s to use them only when absolutely necessary.Research shows MMA can cut opioid use by 32% to 57% without making pain worse. In one study of spine surgery patients, average daily opioid use dropped from 45.2 morphine milligram equivalents (MME) to just 18.7 MME-a 61% reduction. Pain scores stayed under 4 out of 10. That’s not luck. It’s science.
The Core Pillars of MMA
MMA isn’t random. It’s built on proven combinations. Here are the most common and effective pieces:- Acetaminophen (Tylenol): Works centrally to reduce pain signals. Given every 6 hours, IV or oral. Safe for most patients.
- NSAIDs like celecoxib or naproxen: Reduce inflammation at the surgical site. Celecoxib is often preferred because it’s gentler on the stomach. Naproxen is avoided if kidney function is low (eGFR under 30).
- Gabapentin or pregabalin: These calm overactive nerves. Especially helpful after nerve-rich surgeries like spine or joint replacements. Dose must be adjusted for kidney issues.
- Ketamine: A low-dose IV infusion that blocks pain signals in the spinal cord. Used in high-risk patients or those with chronic pain. Can cause dizziness, so it’s monitored closely.
- Lidocaine: An IV infusion that acts like a nerve quieting agent. Proven to reduce pain and opioid needs after major surgeries.
- Dexmedetomidine: A sedative that also reduces pain perception. Often used during surgery and in the first hours after.
These aren’t used in isolation. They’re stacked. For example, a typical spine surgery protocol might start with pre-op acetaminophen, gabapentin, and celecoxib. During surgery, ketamine and lidocaine infusions are added. After surgery, the non-opioid meds continue on a schedule. Opioids? Only for breakthrough pain-and even then, in tiny doses.
Why This Works Better Than Opioids Alone
Opioids only dull pain signals in the brain. They don’t touch inflammation, nerve damage, or muscle spasms. That’s why patients on opioids alone often still hurt-and need more pills. MMA hits pain from all sides.One 2022 review of orthopedic surgeries found that patients on MMA had:
- 41% less opioid consumption
- 28% fewer cases of nausea and vomiting
- Shorter hospital stays (by nearly 2 days in trauma patients)
- Higher rates of same-day discharge
And it’s not just about comfort. Reducing opioid exposure lowers the risk of long-term dependence. Studies now show that patients who get MMA are less likely to still be taking opioids 30 days after surgery. That’s huge.
Who Benefits Most?
MMA works best when pain is predictable. That’s why it’s standard for:- Joint replacements (knee, hip)
- Spine surgeries
- Major orthopedic trauma
- Abdominal surgeries with high pain scores
Even minor surgeries like knee arthroscopy benefit. Opioid use drops by 30-40% with MMA. For patients with chronic pain or opioid tolerance, MMA is even more critical. The Compass SHARP Guidelines recommend adding ketamine, lidocaine, or dexmedetomidine for these high-risk cases.
And yes-some patients ask for opioid-free surgery. It’s possible. With regional nerve blocks, continuous wound infusions of local anesthetics, and the right combo of oral and IV meds, many people can get through recovery without a single opioid pill.
It’s Not Just About Pills
MMA isn’t just drugs. It includes non-drug tools too:- Regional anesthesia: Nerve blocks that numb the surgical area. An ultrasound-guided femoral block for knee surgery? That’s MMA.
- Continuous wound infusion: A small catheter left in the wound that slowly delivers numbing medicine for 2-3 days.
- Physical therapy and movement: Getting up and walking early reduces stiffness and pain.
- Patient education: Telling patients what to expect, how to use their meds, and when to call for help.
One hospital saw same-day discharge rates jump from 12% to 37% just by improving how they communicated pain management plans. Patients who understood their treatment were more confident-and less anxious.
Implementation Isn’t Easy
MMA sounds simple. But putting it into practice? That’s where hospitals struggle. It requires coordination between:- Anesthesiologists
- Surgeons
- Pharmacists
- PACU nurses
- Recovery nurses
- Pre-op nurses
Everyone has to be on the same page. A patient might get gabapentin pre-op, but if the floor nurse doesn’t know to keep giving it after surgery, the whole plan falls apart. That’s why protocols like McGovern Medical School’s use specific order sets in the electronic system-no room for error.
Also, not every hospital can do it. You need ultrasound machines for nerve blocks. You need trained staff. You need policies that require pain scores to be checked every two hours in the first 24 hours. Without that structure, MMA doesn’t stick.

Watch Out for These Pitfalls
MMA is powerful-but it’s not one-size-fits-all. Mistakes happen:- Ignoring kidney function: Gabapentin and naproxen can build up in patients with poor kidney function. Doses must be lowered.
- Stopping meds too soon: Gabapentin shouldn’t be cut off abruptly. Tapering over 5-10 days after discharge helps prevent rebound pain and nerve sensitivity.
- Not assessing mental health: Patients with anxiety or depression often have higher pain sensitivity. They need more support, not just more drugs.
- Overlooking pre-op prep: Giving meds before surgery is key. Waiting until after means you’re already behind.
One hospital reduced opioid use by 60% simply by starting gabapentin and acetaminophen in the pre-op area-not the recovery room.
The Future Is Here
By 2025, experts predict 85% of major surgeries will use formal MMA protocols. That’s up from 60% in 2022. The American Society of Anesthesiologists has made it clear: opioids should be reserved for patients whose pain doesn’t respond to non-opioid options. Not the other way around.The new standard isn’t just about safety. It’s about better outcomes-faster recovery, fewer complications, less addiction, and more patient control. It’s not magic. It’s methodical. And it works.
What You Should Know
If you’re facing surgery:- Ask if your hospital uses multimodal analgesia.
- Find out what non-opioid options they offer.
- Let your team know if you’ve had chronic pain or opioid use in the past.
- Don’t be afraid to ask for a nerve block-it’s safe and effective.
- Take your scheduled meds on time. Don’t wait until you’re in pain.
Recovery doesn’t have to mean dependence. With the right plan, you can heal without opioids.
Is multimodal analgesia only for major surgeries?
No. While it’s most commonly used in major procedures like joint replacements and spine surgery, MMA also works for minor surgeries like arthroscopy or hernia repair. Even in these cases, opioid use drops by 30-40%. The key is consistency-starting non-opioid meds before pain begins, not after.
Can I avoid opioids completely after surgery?
Yes, for many patients. With a strong multimodal plan-including regional nerve blocks, continuous wound infusions, and scheduled non-opioid medications-many people never need an opioid. This is especially true for patients who request opioid-free recovery. Hospitals with dedicated pain teams can design these plans safely and effectively.
Why is gabapentin used in pain management?
Gabapentin doesn’t treat inflammation. It calms overactive nerves that send pain signals after surgery. It’s especially useful for nerve-related pain, like after spine or limb surgeries. Studies show it reduces both pain intensity and opioid needs. Dosing must be adjusted for kidney function-lower doses are needed if eGFR is under 30.
Do I need to take these meds after I leave the hospital?
Yes, for some. Many protocols now include a 5- to 10-day course of gabapentin or similar drugs after discharge. This helps prevent nerves from becoming hypersensitive and reduces the chance of developing chronic pain. Always follow your care team’s instructions-even if you feel fine.
What if I have kidney problems?
Your medication plan will be adjusted. Naproxen is avoided if kidney function is low (eGFR under 30). Gabapentin doses are cut in half or given once daily. Acetaminophen is safe, but always inform your team about your kidney history so they can choose the right options.
Is MMA more expensive than using opioids alone?
Not in the long run. While some non-opioid drugs cost more upfront, the savings come from shorter hospital stays, fewer complications, less need for readmission, and reduced long-term opioid dependence. One hospital saved nearly $2,000 per patient by cutting length of stay by 1.8 days. The cost of pain management is not just in pills-it’s in recovery time.





