Celiac Disease: Understanding the Condition
When you hear celiac disease, a chronic autoimmune disorder triggered by gluten that damages the small intestine. Also known as celiac sprue, it affects millions worldwide. Another key player is the gluten‑free diet, a dietary approach that eliminates wheat, barley, and rye to stop the immune reaction. Accurate diagnostic testing, blood serology and intestinal biopsy used to confirm the disease is essential for proper management.
Why Symptoms Matter
Most people think celiac disease only causes stomach pain, but the reality is broader. Common signs include chronic diarrhea, bloating, fatigue, and unexplained weight loss. Some patients experience skin rashes, joint pain, or anemia. celiac disease can masquerade as other conditions, which is why paying attention to subtle cues is crucial. Recognizing these patterns early can prevent long‑term damage and improve quality of life.
When the immune system attacks the tiny finger‑like villi lining the small intestine, nutrient absorption drops dramatically. This loss can lead to deficiencies in iron, calcium, vitamin D, and B12, worsening fatigue and bone health. Understanding that the gut lining is the main target helps explain why symptoms can be so varied and why a strict diet often brings rapid relief.
Doctors rely on two main pillars for diagnosis: serology tests that detect specific antibodies and an endoscopic biopsy that shows villous atrophy. The presence of anti‑tTG IgA or anti‑EMA antibodies is a strong indicator, but false negatives happen, especially in people with IgA deficiency. In such cases, a duodenal biopsy remains the gold standard. Knowing the strengths and limits of each test guides both patients and clinicians toward accurate results.
Once diagnosed, the cornerstone of treatment is the gluten‑free diet. This means avoiding any food containing wheat, barley, rye, or their derivatives. Modern food labeling laws make it easier to identify safe products, yet hidden sources of gluten still exist in sauces, soups, and processed meats. Learning to read ingredient lists and asking about cross‑contamination in restaurants are practical steps that empower patients.
Adopting a gluten‑free lifestyle can feel daunting, but many resources simplify the transition. Certified dietitians can create personalized meal plans that ensure balanced nutrition while eliminating gluten. Mobile apps now scan barcodes for gluten content, and support groups offer real‑world tips on grocery shopping, dining out, and travel. The goal is to make the diet sustainable, not restrictive.
Untreated celiac disease isn’t just uncomfortable—it can lead to serious complications. Chronic inflammation raises the risk of osteoporosis, infertility, neurological disorders, and even certain cancers like intestinal lymphoma. Monitoring bone density, vitamin levels, and regular follow‑up appointments helps catch these issues early. The long‑term benefit of strict dietary adherence extends far beyond symptom relief.
Research is steadily uncovering new aspects of celiac disease, from genetic markers that predict severity to potential therapies like enzyme supplements that break down gluten before it triggers an immune response. While the gluten‑free diet remains the only proven treatment, staying informed about emerging options keeps patients hopeful and engaged in their health journey.
Below you’ll find a curated collection of articles that dive deeper into every facet mentioned here—symptom checklists, step‑by‑step guides for testing, meal planning ideas, and the latest research updates. Use these resources to build a solid foundation for managing celiac disease confidently.
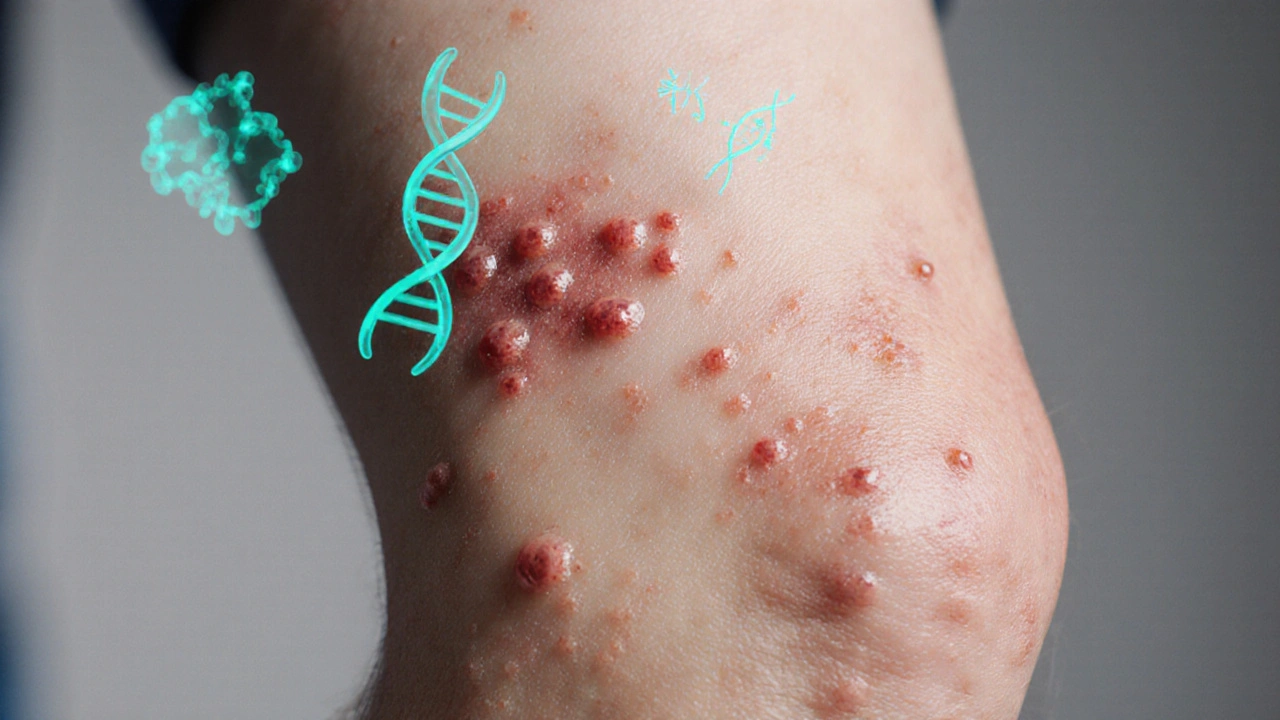
How Genetics Drive Dermatitis Herpetiformis: What You Need to Know
Explore how genetics, especially HLA-DQ2/DQ8, drive dermatitis herpetiformis, its link to celiac disease, testing, family risk, and management.
Read