DH Genetic Risk Calculator
Personal Risk Assessment
Dermatitis Herpetiformis (DH) is strongly linked to specific genetic markers (HLA-DQ2/DQ8) and family history. This calculator estimates your personal risk based on your genetic and family background.
Risk Assessment Results
Next steps:
Key Takeaways
- Dermatitis herpetiformis (DH) is tightly linked to specific HLA genes, especially HLA‑DQ2 and HLA‑DQ8.
- These genes are the same ones that predispose people to celiac disease, making DH essentially a skin manifestation of gluten‑driven autoimmunity.
- Family history matters: first‑degree relatives have a markedly higher chance of developing DH or celiac disease.
- Genetic testing can confirm risk, but diagnosis still relies on skin biopsy and IgA‑based blood tests.
- Lifelong gluten‑free diet and regular follow‑up are the cornerstone of management, with genetics guiding counseling and screening of relatives.
When it comes to skin conditions, Dermatitis Herpetiformis is a chronic, intensely itchy blistering rash that often signals an underlying gluten‑related disorder. Most people think of DH as just a skin problem, but the truth runs deeper: the rash is a visible clue that your immune system is reacting to gluten because of a genetic setup you inherit. Understanding that genetic backdrop helps doctors pinpoint the cause, decide who should be screened, and give patients a clear road‑map for treatment.
In this article we’ll break down the genetics behind DH, explore how those genes interact with gluten, and show you what the latest testing and counseling strategies look like in 2025. By the end you’ll know why a simple blood test isn’t enough, how family history changes your odds, and what steps you can take if you or a loved one is at risk.
What is Dermatitis Herpetiformis?
Dermatitis herpetiformis (DH) presents as clusters of small, raised bumps (papules) and tiny blisters that itch fiercely. They most often appear on elbows, knees, buttocks, and the scalp. The lesions are symmetrical, meaning they show up on both sides of the body. Though the rash looks like a purely dermatological issue, research consistently shows that DH is linked to the same autoimmune mechanisms that cause celiac disease. In fact, up to 90% of DH patients test positive for intestinal damage typical of celiac disease, even if they have no obvious gut symptoms.
The Genetic Blueprint: HLA‑DQ2 and HLA‑DQ8
The strongest genetic signal for DH comes from the human leukocyte antigen (HLA) system, especially the classII molecules HLA‑DQ2 (encoded by the DQA1*05:01/DQB1*02:01 haplotype) and HLA‑DQ8 (DQA1*03:01/DQB1*03:02). These molecules sit on the surface of antigen‑presenting cells and decide which protein fragments get shown to T‑cells.
HLA‑DQ2 is a heterodimeric protein that presents gluten‑derived peptides to CD4+ T‑cells, triggering an immune cascade. About 95% of DH patients carry at least one copy of the DQ2‑encoding genes. The second most common culprit is HLA‑DQ8 which can substitute for DQ2 in presenting gluten peptides, though it appears in a smaller fraction of patients (≈5%). If you lack both DQ2 and DQ8, the chance of developing DH drops to less than 0.1%-a key fact doctors use to rule out the disease.
These HLA genes are not disease‑causing on their own. They create a permissive environment where gluten peptides can stick around long enough to be recognized as foreign. The real damage happens when the immune system starts producing IgA antibodies that target the enzyme tissue transglutaminase (tTG) in the skin. Those antibodies form immune complexes that deposit at the tips of dermal papillae, leading to the characteristic rash.

Beyond HLA: Other Genetic Players
While HLA‑DQ2/DQ8 account for roughly 40% of the heritability, genome‑wide association studies (GWAS) have uncovered additional loci that tweak the risk. Notable examples include:
- STAT4 a transcription factor linked to heightened Th1 immune responses.
- IL2/IL21 genes that regulate cytokine signaling and B‑cell activation.
- SH2B3 a negative regulator of immune cell proliferation, where loss‑of‑function variants increase autoimmunity.
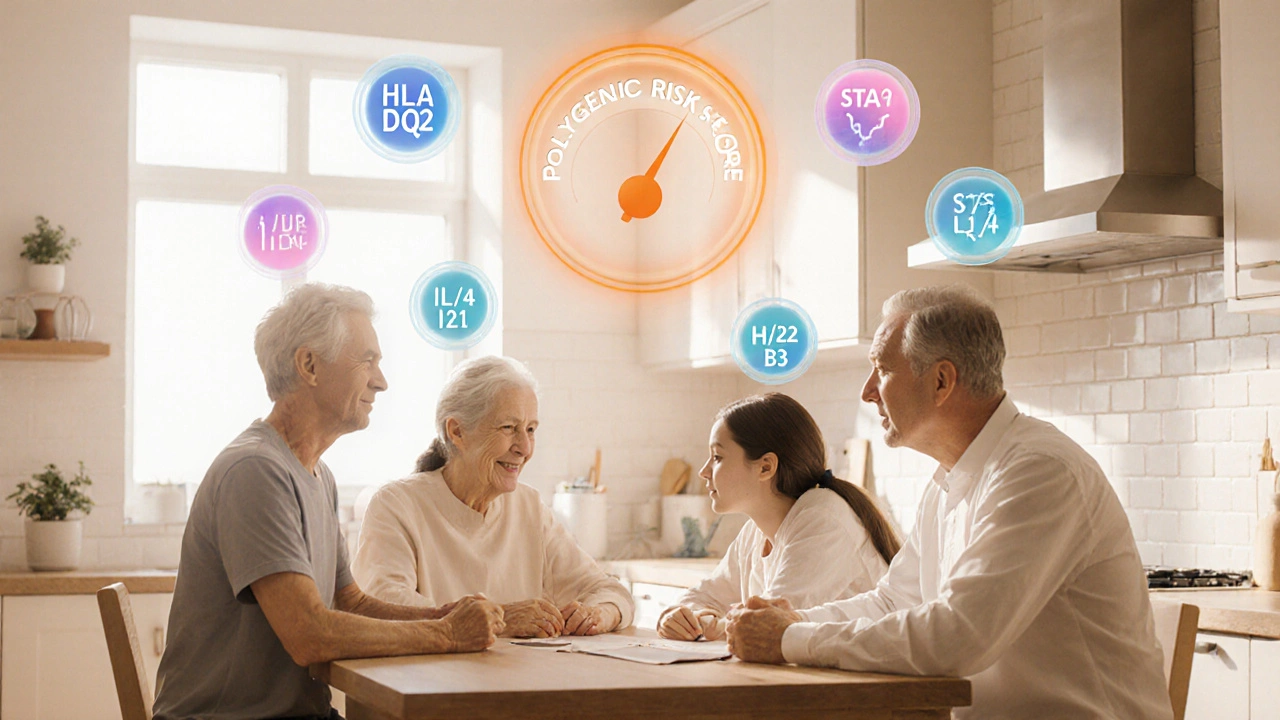
These non‑HLA genes each add a modest 5‑15% increase in risk, but when combined with the HLA high‑risk haplotypes they create a genetic “storm” that makes DH much more likely. The emerging picture is one of polygenic susceptibility: a handful of strong HLA drivers plus a suite of smaller effect genes that together determine whether gluten exposure will trigger skin lesions.
How Genetics Translate to Clinical Practice
Because HLA testing is cheap, fast, and widely available, many clinicians now use a two‑step diagnostic algorithm:
- HLA typing: rule‑out DH if both DQ2 and DQ8 are absent (negative predictive value >99%).
- If HLA‑positive, proceed to skin biopsy with direct immunofluorescence for granular IgA deposits, and serology for anti‑tTG IgA and anti‑endomysial antibodies.
Patients who are HLA‑positive but lack skin findings may still develop DH later, especially after periods of increased gluten intake or other immune triggers (e.g., infections, hormonal shifts). This knowledge lets doctors counsel patients about lifelong risk and the benefits of strict gluten avoidance before symptoms even appear.
Family History: Who Should Get Tested?
First‑degree relatives (parents, siblings, children) of a DH patient inherit the HLA haplotypes at a 50% chance. Studies from the European Celiac Disease Registry in 2023 report that among families where one member has DH, 12% of relatives develop DH or celiac disease within ten years, compared with 1% in the general population.
Practical guidance:
- Ask every DH patient for a detailed family history of skin rashes, chronic diarrhea, or unexplained anemia.
- If a relative is HLA‑positive, recommend baseline serology (anti‑tTG IgA) even if they feel fine.
- Encourage at‑risk relatives to adopt a gluten‑free diet only if serology turns positive-unnecessary restriction can affect quality of life.
Genetic Testing: What’s Available in 2025?
Two main options dominate the market:
| Provider | Method | Turn‑around | Cost (UK) | Coverage |
|---|---|---|---|---|
| Genomics UK | High‑resolution NGS | 3‑5 days | £85 | DQ2, DQ8, rare alleles |
| HealthCheck Labs | PCR‑based typing | 1‑2 days | £55 | DQ2, DQ8 only |
| Direct to Consumer (e.g., MyGenome) | Microarray | 7‑10 days | £70 | DQ2, DQ8 + limited SNP panel |
High‑resolution NGS gives the most complete picture, catching rare HLA sub‑types that may affect disease severity. For most clinical scenarios, the PCR‑based test is adequate because the primary question is “Do you have DQ2 or DQ8?”.
Implications for Treatment and Lifestyle
Once the genetic and serologic work‑up is complete, the cornerstone of therapy is a strict gluten‑free diet (GFD). Unlike celiac disease where intestinal healing may take months, DH skin lesions often improve within weeks of eliminating gluten. Some patients also need a short course of dapsone to control itching while the diet takes effect.
Genetics influence two practical aspects of management:
- Risk stratification: HLA‑DQ2 homozygotes tend to have higher anti‑tTG titers and may need more vigilant monitoring for complications such as osteoporosis.
- Family counseling: Knowing that a sibling carries the same HLA risk can prompt early serologic screening, potentially catching celiac disease before it causes bone loss.
Future Directions: Polygenic Risk Scores (PRS)
Researchers are now building PRS that merge HLA status with the smaller‑effect genes (STAT4, IL2/IL21, SH2B3, etc.). A 2024 pilot in the UK showed that a PRS >0.85 correctly identified 78% of patients who later developed DH, compared with 55% using HLA alone. While PRS isn’t yet standard care, it promises a more nuanced prediction model that could guide personalized diet recommendations and timing of skin biopsies.
Key Points to Remember
- Genetics set the stage: without HLA‑DQ2 or DQ8, DH is virtually impossible.
- The same genes that drive celiac disease also drive DH - think of the rash as a skin echo of a gut problem.
- Family history dramatically raises risk; screening relatives can catch disease early.
- HLA testing is a quick, cost‑effective first step that rules out DH in >99% of negative cases.
- A lifelong gluten‑free diet, supported by dietitian advice, is the most effective treatment.
Frequently Asked Questions
Can I develop dermatitis herpetiformis if I don’t have celiac disease?
Yes. Although up to 90% of DH patients show intestinal damage typical of celiac disease, a small minority have normal gut biopsies. The common denominator is still the presence of HLA‑DQ2 or DQ8 and an IgA response to gluten.
If I test negative for HLA‑DQ2/DQ8, is there any chance I could still get DH?
The risk is exceedingly low-studies report a false‑negative rate of less than 0.1%. In clinical practice a negative HLA test essentially rules out DH, and physicians will look for other diagnoses.
Should my children be tested for HLA‑DQ2/DQ8 if I have DH?
Testing children is optional. If a child is HLA‑positive, regular serology every few years can catch early celiac changes. Immediate gluten restriction isn’t recommended unless serology becomes positive.
How long does it take for the rash to clear after starting a gluten‑free diet?
Most patients notice itching reduction within 2‑4 weeks, and visible lesions fade within 2‑3 months. Dapsone can speed up symptom relief during the first few weeks.
Are there any new therapies beyond the gluten‑free diet?
Research on transglutaminase‑targeted monoclonal antibodies is ongoing, but none are approved yet. For now, diet and, when needed, dapsone remain the standard of care.






Comments
Alec McCoy
12/Oct/2025Hey folks, let’s dive into this fascinating world of genetics and dermatitis herpetiformis together. The way HLA‑DQ2 and DQ8 set the stage is like a backstage pass to an exclusive concert you didn’t even know you were invited to. First, remember that genetics is not destiny; it’s a roadmap that can be rerouted with lifestyle choices, especially diet. If you have a family history, think of it as having a GPS that already points toward a higher‑risk zone, but you can still take alternate routes. Understanding your risk empowers you to make proactive decisions, like getting tested early and adopting a gluten‑free lifestyle before the rash even appears. The calculator in the article is a handy tool, but it’s the conversation with your doctor that turns numbers into actionable steps. Don’t let the jargon intimidate you-HLA‑DQ2 means a specific protein that presents gluten fragments, and DQ8 is its cousin, both acting like overly enthusiastic bouncers at the gut‑skin gate. When those bouncers get over‑excited, they flag gluten peptides and launch an immune response that ends up in itchy blisters. This process is reversible; many patients see dramatic improvement once gluten disappears from the menu. Keep an eye on your serology; anti‑tTG antibodies are the breadcrumbs that tell you if the immune system is still peeking through. If you’re HLA‑positive but asymptomatic, regular blood work every couple of years is a smart preventive measure. And for those who develop symptoms, a short course of dapsone can fast‑track relief while the diet takes effect. Remember, you’re not alone in this journey-support groups, dietitians, and specialists form a network that can guide you through the ups and downs. Stay curious, stay motivated, and use the genetic information as a compass rather than a verdict. Together we can turn a potentially scary diagnosis into a manageable, even empowering, part of life.
Aaron Perez
12/Oct/2025Consider, if you will, the existential implication of HLA markers; they are not merely molecular sequences, they are the silent architects of fate; thus the rash becomes a manifesto of our genomic arrogance, a reminder that the genome conspires with environment in a dance of inevitability; yet we, the observers, stand bewildered, clutching calculators as if they were talismans against the inexorable march of autoimmunity; what does it mean when a tissue transglutaminase becomes the unwilling messenger? It is a paradox, a betrayal of the body’s own chemistry, and it beckons us to question the very nature of self; perhaps the true horror lies not in the itch, but in the realization that our genetic inheritance scripts our suffering, echoing a cosmic joke that we cannot escape.
William Mack
12/Oct/2025Great info! The HLA stuff can feel like a maze, but the key takeaway is that testing helps narrow it down fast. If you’re positive, keep an eye on symptoms and get regular blood work.
Evan Riley
12/Oct/2025Listen, these labs are part of a hidden agenda. Big pharma loves you to stay on meds like dapsone forever while they market gluten‑free substitutes as a cash grab. The real cure is out there, they’re just keeping it under wraps. Stay skeptical and demand more transparency about the long‑term effects of these diets.
Nicole Povelikin
12/Oct/2025i dont see why every1 has to get tested, its overhyped. sure dna can be a thing but i think its just a fad, plus my aunt says gluten is fine for her. maybe we are all just anxious about normal stuff.
Michelle Weaver
12/Oct/2025For anyone seeking clarity, the step‑wise approach-HLA typing, followed by serology and biopsy-provides a robust diagnostic pathway. It minimizes unnecessary interventions and guides precise management. 😊
John Keough
12/Oct/2025I appreciate the thorough breakdown; it demystifies a complex topic. Balancing the scientific details with practical advice makes it accessible. Let’s keep the conversation focused on evidence and supportive care.
Graham Smith
12/Oct/2025The article contains a few typos – ‘thoroughly’ is misspelled, and there’s an inconsistent use of the Oxford comma. Minor errors, but they can distract from the content.
Jeremiah Morgan
12/Oct/2025Thank you for pointing out those details; precision matters in scientific communication. Your vigilance helps maintain high standards that benefit all readers.
nina greer
12/Oct/2025The discourse here merely scratches the surface of immunogenetics.
Montague Tilmen
12/Oct/2025We should prioritize American research over foreign clinics; our own labs can handle the testing without outsourcing.
Clarise Wheller
12/Oct/2025While supporting domestic science is important, collaboration across borders often accelerates breakthroughs. Let’s stay open to global expertise.
Riley Fox
12/Oct/2025Indeed-cross‑border cooperation, when harnessed wisely, can yield synergistic outcomes; however, vigilance is required to ensure data integrity, consent, and equitable benefit sharing; the future lies in balanced partnerships 🌍😉.
Adam Craddock
12/Oct/2025Could the emerging polygenic risk scores eventually replace single‑gene HLA testing for dermatitis herpetiformis risk stratification? Further longitudinal studies will clarify their clinical utility.