AGEP Risk Assessment Tool
AGEP Risk Assessment Tool
Assess your risk of developing Acute Generalized Exanthematous Pustulosis (AGEP) from medications. Identify high-risk drugs and get guidance on next steps.
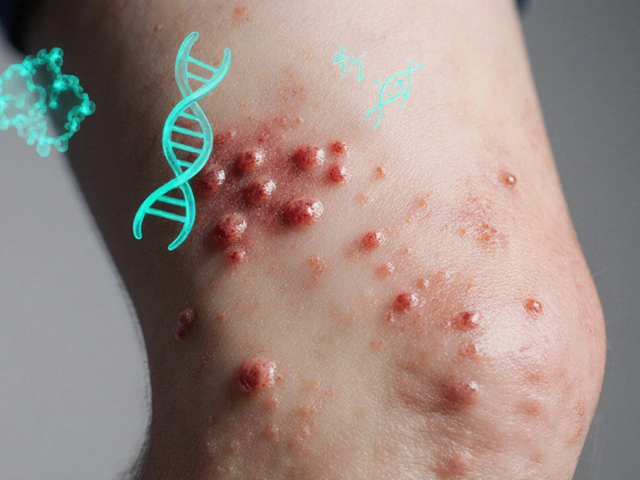
Imagine waking up with your skin covered in tiny white bumps, burning hot, and covered in redness - all within a day or two after taking a common antibiotic. This isn’t a fungal infection or acne. It’s Acute Generalized Exanthematous Pustulosis (AGEP), a rare but serious drug reaction that can turn your life upside down in under 48 hours.
What Exactly Is AGEP?
AGEP is a sudden, severe skin reaction triggered by medications. It’s not contagious, not allergic in the classic sense, and not psoriasis - though it looks similar. The hallmark? Hundreds of small, sterile pustules (not filled with bacteria) that pop up on a red, inflamed base. They start in skin folds - armpits, groin, neck - then spread fast. Within two days, they can cover most of your body.
First identified in 1980, AGEP affects about 1 to 5 people per million each year. That’s rarer than lightning strikes. But when it hits, it hits hard. It’s most common in adults, with no big difference between men and women. Kids can get it too, but it’s uncommon.
What makes AGEP dangerous isn’t just how it looks - it’s how quickly it can mimic other life-threatening conditions like Stevens-Johnson Syndrome or generalized pustular psoriasis. Misdiagnosis happens in 35-40% of cases outside specialized dermatology centers. That’s why knowing the signs matters.
How Does AGEP Start?
Almost all cases - over 90% - are caused by drugs. The usual suspects? Antibiotics. Specifically, amoxicillin-clavulanate (Augmentin), erythromycin, and other beta-lactams. But it’s not just antibiotics. Antifungals, calcium channel blockers, and even some NSAIDs can trigger it.
The timing is telling. Symptoms usually show up 1 to 5 days after taking the drug - often around day two. But with amoxicillin-clavulanate, it can take up to 14 days. That delay tricks people into thinking the drug is safe. It’s not.
Once the reaction starts, it races. Fever? Common. White blood cell count through the roof? Almost always. Neutrophils - the body’s first responders - spike to over 75% of total white cells. CRP, a marker of inflammation, jumps too. These aren’t just lab numbers. They’re your body screaming that something’s wrong.
How Is AGEP Different From Psoriasis?
This is where things get tricky. Generalized pustular psoriasis looks nearly identical under the microscope. But here’s the difference:
- AGEP pustules appear suddenly after a drug. Psoriasis pustules flare without a clear trigger.
- AGEP rarely affects palms and soles. Psoriasis often does.
- AGEP resolves in 10-14 days after stopping the drug. Psoriasis is chronic.
- AGEP has a 2-4% mortality rate. Generalized pustular psoriasis? Up to 25%.
That’s why a biopsy and careful history matter. A skin sample showing subcorneal pustules with neutrophils and eosinophils is classic AGEP. No fungi, no bacteria - just your immune system overreacting.
What Should You Do If You Suspect AGEP?
Stop the drug. Immediately. That’s the single most important step. No exceptions. Even if you think it’s "just a rash," don’t wait. Every hour counts.
Next: get to a hospital. If you have a fever over 38.5°C, widespread rash, or feel dizzy or weak, you need to be admitted. Average hospital stays run 5.7 to 9.3 days. Why? Because AGEP can affect your kidneys, liver, or lungs. Monitoring isn’t optional - it’s life-saving.
Supportive care is the foundation:
- Moist dressings to soothe raw skin
- Topical steroids for itch and inflammation
- Antihistamines if you’re scratching raw
- Fluids and electrolytes if you’re losing fluids through peeling skin
And after the rash fades? You’ll peel. That’s normal. It’s called desquamation. It starts around day 7 and can last a week. Use thick emollients. Avoid sun. Your new skin is fragile.

The Big Debate: Should You Use Steroids?
This is where doctors disagree - and it matters for your care.
Some experts - including dermatologists from Baylor College of Medicine - say no to systemic steroids. Their argument? AGEP clears on its own. Steroids add risk: high blood sugar, mood swings, infection risk. In their 3-year experience with 15 cases, patients recovered fine without them.
But other experts - including a European panel - say yes, especially if the rash covers more than 20% of your body or you’re very sick. A 2023 study showed 87% of steroid-treated patients improved in 7 days, compared to 63% without. Steroids cut hospital stays by over 3 days.
So what’s the answer? It’s not black and white. The latest review from 27 dermatologists across 15 countries says: individualize the decision. If you’re elderly, diabetic, or have heart disease, steroids might be too risky. If you’re young, otherwise healthy, and covered in pustules, they could speed recovery.
What If Steroids Don’t Work - Or Can’t Be Used?
There are other options. One is cyclosporine - an immune suppressant used in organ transplant patients. At 3-5 mg per kg per day, it works as well as steroids but with fewer metabolic side effects.
Even more promising? Biologics. Secukinumab, a drug used for psoriasis and arthritis, targets IL-17 - a key player in AGEP inflammation. In one case, a patient who couldn’t take steroids got secukinumab and was clear in 72 hours. Another patient saw results in under 48 hours.
These aren’t first-line treatments - yet. But they’re becoming lifelines for people who don’t respond to standard care. Clinical trials are underway. Early results show 92% effectiveness with minimal side effects.
What Drugs Are Most Likely to Cause AGEP?
Not all drugs are equal. Here’s what the data shows:
- Antibiotics (56%): Amoxicillin-clavulanate tops the list. Macrolides like erythromycin and clarithromycin are next.
- Antifungals (12%): Fluconazole and terbinafine are common triggers.
- Calcium channel blockers (8%): Diltiazem and amlodipine can cause it.
- Others: Paracetamol, ibuprofen, and even some anticonvulsants have been linked.
Regulatory agencies now require drug labels to list AGEP as a potential side effect. Amoxicillin-clavulanate got a warning update in 2021 after 127 confirmed cases were reported in Europe. That’s progress.

What’s Next for AGEP?
Science is catching up. The EuroSCAR group is rolling out a new diagnostic tool called AGEP 2.0 - a scoring system that’s 94% accurate at spotting true cases. That’s huge for community hospitals where misdiagnosis is common.
Genetic research is also moving fast. A specific gene variant - HLA-B*59:01 - is linked to higher AGEP risk in Asian populations. Odds of developing it if you carry this gene? Nearly 9 times higher. That could lead to pre-screening before prescribing high-risk drugs.
And the future? Personalized medicine. Imagine getting a blood test before starting antibiotics that tells you if you’re genetically at risk. That’s not sci-fi - it’s coming.
What Should You Do After Recovery?
Once you’re healed, you need to know what caused it - and avoid it forever. Keep a written list of the drug(s) you reacted to. Share it with every doctor you see. Put it in your phone’s health app. Tell your pharmacist.
Studies show patients who get written instructions after AGEP are twice as likely to avoid the trigger again. Verbal advice? Only 42% remember it correctly. Written? 78%.
Also, don’t assume all drugs in the same class are safe. If amoxicillin-clavulanate caused AGEP, avoid all penicillin derivatives. Cross-reactivity is real.
Final Thoughts
AGEP is rare, but it’s not rare enough to ignore. It’s fast. It’s painful. It can be deadly if mismanaged. But with quick action, it’s also highly treatable. The key is recognizing it early - and stopping the drug before it spirals.
If you’ve had a sudden rash after a new medication - especially with fever and pustules - don’t wait. Don’t reach for hydrocortisone cream and hope it goes away. Go to urgent care. Go to the ER. Tell them: "I think I might have AGEP."
Your skin might heal. But your life depends on getting the right diagnosis - fast.
Can AGEP come back if I take the same drug again?
Yes - and it will likely be worse. Once you’ve had AGEP from a specific drug, your immune system remembers it. Re-exposure can trigger a more severe reaction, sometimes within hours. Avoid the drug completely and all related medications. Keep a written list and share it with every healthcare provider.
Is AGEP contagious?
No. AGEP is not caused by bacteria, viruses, or fungi. It’s a reaction inside your own immune system. You cannot spread it to others through touch, air, or bodily fluids. There’s zero risk of transmission.
How long does AGEP last?
Without treatment, most cases clear in 10 to 14 days after stopping the triggering drug. With supportive care and sometimes steroids, improvement can start in 3-5 days. Full skin recovery, including peeling, takes about 2-3 weeks. Long-term scarring is rare.
Can children get AGEP?
Yes, though it’s uncommon. Children account for less than 10% of reported cases. When they do get it, antibiotics - especially amoxicillin - are the usual trigger. Symptoms and treatment are similar to adults, but dosing must be adjusted for weight. Pediatricians should consider AGEP in any child with sudden pustules and fever after starting a new medication.
Are there any long-term health risks after AGEP?
Most people recover fully with no lasting effects. But some studies suggest a slightly higher risk of developing autoimmune conditions later, like psoriasis or thyroid disease - though the link isn’t proven. The biggest long-term risk is accidental re-exposure to the triggering drug. That’s why documenting and avoiding the culprit is critical.
Can I take other antibiotics after having AGEP?
Maybe - but not the same class. If amoxicillin caused your AGEP, avoid all penicillins and cephalosporins unless tested by an allergist. Other classes like macrolides (azithromycin) or tetracyclines (doxycycline) are often safe, but always check with your doctor. Never self-prescribe antibiotics after AGEP. Your risk of another reaction is higher than average.





Comments
Stacy Thomes
22/Jan/2026This happened to my sister last year after she took Augmentin for a sinus infection. One day she was fine, the next she looked like she’d been boiled alive. We rushed to the ER and they didn’t even know what it was at first. Don’t wait. If you get a sudden rash with fever after a new med? GO. NOW.
dana torgersen
22/Jan/2026okay so like… i just read this and… wow… i mean… like… i’ve had a rash before… and i thought it was just… like… heat… or… stress… but… what if… what if it was AGEP?? and i didn’t know?? and i kept taking the meds?? and then… what if… i died??
Janet King
22/Jan/2026AGEP is a well-documented adverse drug reaction with a clear diagnostic pathway. The key clinical indicators are rapid-onset sterile pustules, neutrophilia, and a temporal association with medication exposure. Early discontinuation of the offending agent remains the cornerstone of management. Supportive care is typically sufficient, though systemic corticosteroids may be considered in severe cases with extensive skin involvement.
Vanessa Barber
22/Jan/2026Yeah but have you actually seen the skin? Like… it’s not just ‘rash’. It’s like someone poured boiling sugar on a baby and then left it out in the sun. I’ve seen it. It’s not ‘mild’. Stop acting like it’s just a bad case of acne.
Susannah Green
22/Jan/2026My dermatologist told me to always keep a drug reaction log-paper copy, phone note, even a sticker on my wallet. After my AGEP, I avoided every penicillin for 5 years. Then I got a UTI and my PCP prescribed amoxicillin again. I had to call her at midnight and scream. She apologized. Now she keeps my file flagged. Don’t trust memory. Write it down.
Anna Pryde-Smith
22/Jan/2026They’re still prescribing amoxicillin-clavulanate like it’s candy. This isn’t rare-it’s ignored. Hospitals don’t train residents on AGEP because it’s ‘rare’. But when it hits you? It’s the most terrifying thing you’ll ever feel. The skin burns. The fever won’t break. And no one takes you seriously until you’re in ICU. Wake up, medical system.
Oladeji Omobolaji
22/Jan/2026Man, I just read this and I’m thinking-this is why I never take antibiotics unless I really need them. Back home in Nigeria, we use herbs for coughs. Maybe that’s why I never got this. But I know people who died from ‘just a rash’. This post? It’s a warning. Share it.
Laura Rice
22/Jan/2026To anyone reading this: if you’ve ever had a weird rash after meds, even if it went away-you need to talk to your doctor. Don’t be embarrassed. Don’t think it’s ‘not a big deal’. I had a mild one after a Z-pack and thought nothing of it. Two years later? Full AGEP from amoxicillin. I wish I’d listened to my gut. You’re not overreacting. Your body is screaming.
charley lopez
22/Jan/2026The pathophysiology of AGEP involves IL-17-mediated neutrophilic infiltration of the epidermis, triggered by haptenization of drug metabolites with keratinocyte proteins. The diagnostic gold standard remains histopathological confirmation of subcorneal pustules with neutrophilic predominance and absence of microbial organisms. Differential diagnosis requires exclusion of SJS/TEN, pustular psoriasis, and infectious pustulosis.
Sallie Jane Barnes
22/Jan/2026My son was 7 when he got AGEP from amoxicillin. We were in the ER for 5 days. He didn’t speak for 3 days-he was too scared. The nurses gave him ice pops and read him Harry Potter. We didn’t know what was happening. But we learned. Now his school has his drug allergies on file. His teacher knows. His coach knows. We made sure. Don’t let fear silence you. Speak up.
Andrew Smirnykh
22/Jan/2026In some cultures, people avoid hospitals unless absolutely necessary. This post is a bridge. For those who’ve never heard of AGEP, it’s not just a medical term-it’s a life sentence if ignored. Thank you for writing this with such clarity. I’m sharing it in my community group. Knowledge saves lives.
Kerry Evans
22/Jan/2026People who say ‘just stop the drug’ are being naive. What if you’re on it for a life-threatening infection? What if the doctor insists it’s ‘just a rash’? You don’t just ‘stop’ antibiotics when you’re septic. This isn’t a checklist-it’s a minefield. And the medical system still treats patients like they’re dumb for not knowing this.
Kerry Moore
22/Jan/2026I’m a pharmacist. I’ve seen this too many times. Patients come in with a rash and say, ‘I think it’s the new pill.’ We check the list-amoxicillin-clavulanate, 87% of the time. We warn them. But they say, ‘It’s just a little red.’ I wish I could hand every patient this article. Please, if you’re on antibiotics and develop a rash-stop. Call your doctor. Don’t wait until you’re burning up.
Sue Stone
22/Jan/2026I had this. Took 3 weeks to heal. Peeling for days. Felt like I was shedding skin like a snake. The worst part? No one believed me. My boss thought I was faking to get out of work. I quit. Never going back to a job that doesn’t take your health seriously.
Dawson Taylor
22/Jan/2026AGEP is a sentinel event. It reveals systemic gaps in drug safety education. The real tragedy isn’t the disease-it’s that we don’t screen for genetic risk before prescribing. HLA-B*59:01 testing should be routine in high-risk populations. Prevention beats treatment every time.