Finding clumps of hair in your brush and a flaky scalp can feel like a double whammy. While dandruff or stress often get blamed, a hidden fungal infection might be the real culprit. Understanding how a scalp fungus triggers hair loss helps you spot the warning signs, get the right tests, and choose an effective cure.
Key Takeaways
- Scalp fungal infections, especially tinea capitis, are a common cause of patchy hair loss.
- Dermatophytes and Candida species invade hair follicles, leading to inflammation and breakage.
- Diagnosis relies on visual clues, Wood's lamp examination, microscopy, and culture.
- Oral antifungals such as terbinafine or itraconazole are the most reliable treatments; topical agents help reduce spread.
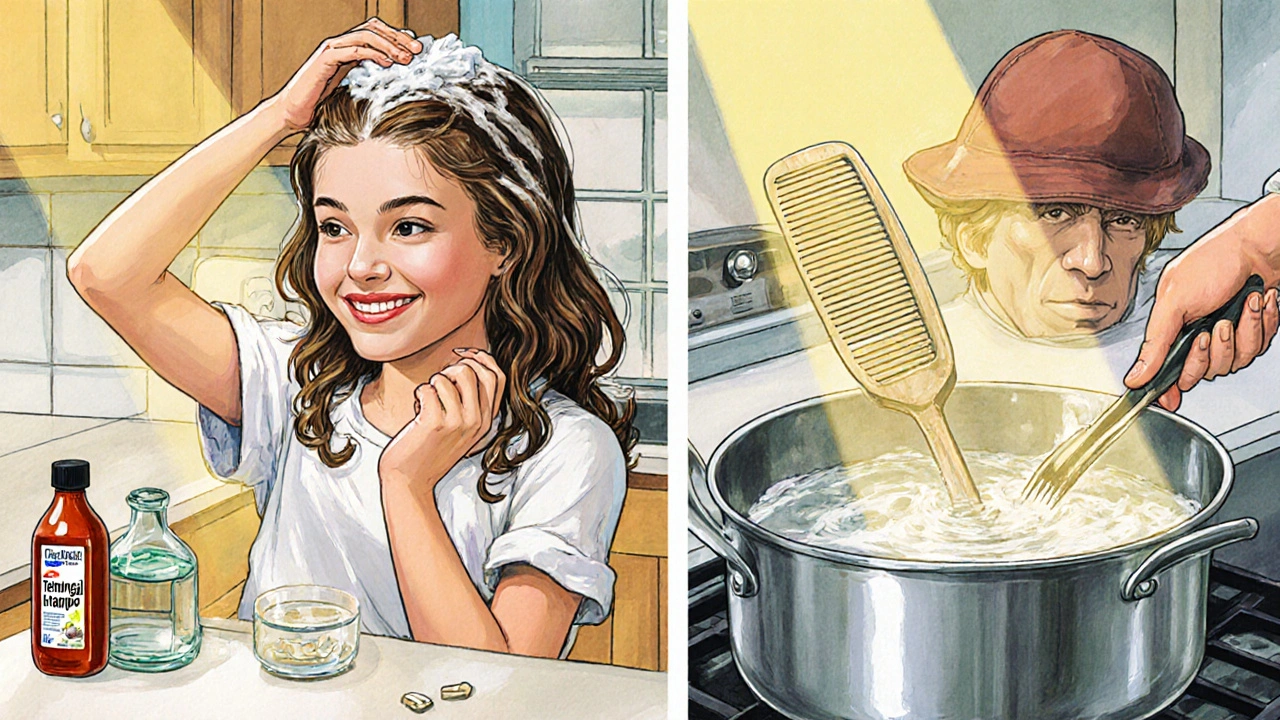
- Good hygiene, avoiding shared combs, and keeping the scalp dry can prevent re‑infection.
Below, we break down everything you need to know from the biology of the fungus to practical steps for recovery.
What Is a Scalp Fungal Infection?
Tinea capitis is a contagious fungal infection of the scalp caused primarily by dermatophyte species such as Trichophyton tonsurans and Microsporum canis. It most often affects children aged 5‑15, but adults with compromised immunity or poor scalp hygiene can develop it as well. The fungus feeds on keratin, the protein that makes up hair and the outer skin layer, allowing it to colonize hair shafts and follicles.
Another term you may hear is "scalp ringworm" - a lay‑person label for the same condition. Despite the name, no worm is involved; it’s the fungus that creates the characteristic circular patches.
How Fungi Lead to Hair Loss
When dermatophytes invade a hair follicle, they produce enzymes that break down keratin. This weakens the hair shaft, causing it to become brittle and break near the scalp. In addition, the body’s immune response triggers inflammation, which can damage the follicle’s root and temporarily halt the growth cycle.
In severe cases, the infection causes "black dot" hair loss - tiny black specks where hair shafts break off at the scalp surface. Over time, the patch can enlarge, leaving a visibly bald area.
Common Fungal Species Involved
- Dermatophyte is a group of fungi that feed on keratin and cause skin, nail and hair infections. The most frequent culprits on the scalp are Trichophyton tonsurans (endothrix - growing inside the hair shaft) and Microsporum canis (ectothrix - surrounding the shaft).
- Candida albicans is a yeast that can opportunistically infect the scalp, especially in people with oily skin or after long‑term antibiotic use. Unlike dermatophytes, Candida tends to cause moist, eczema‑like patches and may coexist with other scalp conditions.

Distinguishing Fungal Hair Loss from Other Causes
Hair loss can stem from many factors - hormonal changes, autoimmune disorders, stress, or nutritional deficiencies. Here’s how fungal‑related loss stands out:
- Patchy, well‑defined bald spots with scaling or crusted lesions.
- Presence of black dots (broken hair shafts) or gray patches where hairs have fallen out.
- Often accompanied by itching, burning, or a foul odor.
- History of contact with infected individuals or shared items (hats, combs).
If you notice smooth bald areas without scaling, or diffuse thinning across the crown, a fungal infection is less likely and you may be dealing with androgenetic alopecia or telogen effluvium instead.
Diagnosis: From Observation to Lab Tests
Because early symptoms mimic dandruff or eczema, a clinician uses a stepwise approach:
- Visual examination: Identifies characteristic ring‑shaped plaques and black‑dot pattern.
- Wood's lamp examination: When you shine a UV light on the scalp, some species (e.g., Microsporum canis) fluoresce bright green. Wood's lamp is a diagnostic tool that emits ultraviolet light to highlight certain fungal infections.
- Microscopic examination: A scalp scraping examined with a potassium hydroxide (KOH) prep reveals hyphae or spores. Microscopic examination is a lab technique that visualizes fungal elements in skin or hair samples.
- Culture: Placing the sample on Sabouraud agar for 1‑2 weeks confirms the exact species, guiding treatment choice.
These tests together give a definitive answer, allowing you to avoid unnecessary hair‑loss treatments that target hormonal or autoimmune causes.
Treatment Options: Getting the Fungus Out
The backbone of therapy is an oral antifungal. Topical agents help reduce surface spread but can’t reach the hair shaft where the fungus lives.
| Medication | Form | Typical Duration | Key Benefits | Side‑effects |
|---|---|---|---|---|
| Terbinafine | Oral tablets | 4‑6 weeks | High cure rate for Trichophyton species | Rare liver enzyme elevation |
| Itraconazole | Oral capsules | 4‑8 weeks (pulse dosing) | Effective against resistant strains | GI upset, drug interactions |
| Ketoconazole | Topical shampoo/cream | 2‑4 weeks + weekly maintenance | Reduces surface fungal load | Skin irritation, rare hormonal effects |
| Miconazole | Topical cream | 2‑3 weeks | Broad‑spectrum, over‑the‑counter | Minimal; occasional itching |
fungal infection hair loss typically clears up within 8‑10 weeks once the course is finished, but you may see new hair growth take a few months as follicles recover.
In addition to medication, clinicians advise:
- Wash hair daily with an antifungal shampoo during treatment.
- Disinfect combs, brushes, hats, and pillowcases with hot water (≥60 °C) or a 10% bleach solution.
- Avoid sharing personal grooming items.
Prevention: Keeping Your Scalp Fungus‑Free
Even after you’ve cleared an infection, the risk of re‑infection remains if habits don’t change. Adopt these simple steps:
- Keep the scalp dry - excess moisture fuels fungal growth. Use a breathable hairdryer on low heat after washing.
- Choose anti‑dandruff shampoos containing zinc pyrithione or selenium sulfide as a maintenance routine.
- Avoid tight headgear that traps sweat; let your hair breathe.
- Screen family members or close contacts for similar lesions; treat them simultaneously.
When to Seek Professional Help
If you notice any of the following, book an appointment promptly:
- Rapidly expanding bald patches or severe itching.
- Signs of secondary bacterial infection - redness, warmth, pus.
- Hair loss that doesn’t improve after two weeks of over‑the‑counter dandruff shampoo.
- History of immune‑suppressing conditions (diabetes, HIV, chemotherapy).
Early treatment shortens the course and reduces the chance of permanent scarring alopecia.
FAQs
Can a fungal infection cause permanent hair loss?
If the infection is treated early, hair usually regrows. Chronic or severe cases can damage follicles permanently, leading to scarring alopecia. Prompt medical care minimizes that risk.
Is tinea capitis contagious?
Yes. It spreads through direct scalp contact, shared hats, combs, or bedding. Children in schools are especially vulnerable.
Do over‑the‑counter shampoos cure scalp fungus?
OTC shampoos (zinc pyrithione, selenium sulfide) help control surface growth but rarely eradicate the fungus within the hair shaft. Oral medication is usually required for cure.
Can adults get tinea capitis?
Adults can develop it, especially if they have weakened immunity, oily scalp, or frequent headgear use. It’s less common than in kids but not rare.
How long does it take for hair to grow back after treatment?
Hair regrowth follows the normal cycle-usually 2‑4 months for visible length, with full thickness restored in 6‑12 months, depending on age and overall health.
Understanding the link between fungal infections and hair loss puts you in control. Spot the signs, get the right tests, and follow an evidence‑based treatment plan. Your scalp will thank you with healthier, fuller hair.






Comments
kenny lastimosa
23/Oct/2025When you look at a stubborn scalp fungus, you realise it's a quiet rebellion of biology against our expectations of health. The fungus thrives on keratin, turning something that protects us into a source of loss. This paradox invites us to consider how often we ignore subtle signs, like a few stray hairs in the brush, until the problem declares itself louder. It's a reminder that the body communicates in whispers before it screams. So, before we dismiss itch or flake, we might pause and ask what hidden ecosystem is at play.
Heather ehlschide
23/Oct/2025One practical way to differentiate a fungal scalp infection from other types of alopecia is to examine the pattern of scaling and the presence of black dots, which are essentially hair shafts broken at the surface. Tinea capitis often manifests as well‑defined, circular plaques that may fluoresce under a Wood's lamp if caused by Microsporum species, whereas androgenetic alopecia presents as diffuse thinning without scaling. A potassium hydroxide (KOH) preparation can reveal hyphae or spores within a few minutes, giving a rapid clue before cultures are ready. Culturing on Sabouraud agar, although slower, allows precise identification of the dermatophyte involved, which can guide the choice between terbinafine and itraconazole. Oral antifungals remain the cornerstone of treatment because topical agents cannot penetrate the hair shaft where the fungus resides. However, adjunctive use of shampoos containing selenium sulfide or zinc pyrithione can reduce surface colonization and lower the risk of reinfection. It is also essential to educate patients about hygiene: regular washing of bedding, hats, and combs in hot water or a bleach solution can break the transmission cycle, especially in households with children. For patients with compromised immunity, such as those with diabetes or on immunosuppressive therapy, a longer course or pulse dosing of itraconazole may be necessary to achieve eradication. Monitoring liver function tests before and during therapy with terbinafine is advisable, even though hepatotoxicity is rare. In cases where secondary bacterial infection occurs, a short course of an appropriate antibiotic may be added to prevent further follicular damage. The timeline for visible regrowth typically follows the normal hair cycle, with new hairs appearing after 2–4 months, and full thickness restoration may take up to a year. Patience and adherence to the medication schedule are key, as premature discontinuation can lead to relapse. Moreover, patients should be warned that over‑the‑counter antifungal shampoos alone are insufficient for cure, as they only address superficial organisms. Finally, follow‑up appointments should include a repeat Wood's lamp examination and possibly a repeat KOH prep to confirm clearance before declaring the infection resolved. Consistent communication with a dermatologist ensures any lingering issues are addressed promptly.
Kajal Gupta
23/Oct/2025Yo, picture those fungal spores as tiny party crashers that sneak into your hair follicles, set up a rave, and then leave a mess of broken strands – that's the "black dot" drama you read about. The good news is that with the right antifungal playlist, you can kick them out and let your hair grow back like a fresh set of fireworks. Think of terbinafine as the headlining DJ, while selenium sulfide shampoos are the backup singers keeping the stage clean. Just don’t forget to wash your combs, because sharing them is like passing the mixtape of infection to the next unsuspecting fan. Stay cool, keep the scalp dry, and let the natural rhythm of hair regrowth do its thing.
Scott Ring
23/Oct/2025I completely agree that a thorough diagnostic work‑up saves a lot of guesswork later on. In my experience, patients who get a KOH prep early feel more confident about sticking to the oral regimen. Also, reminding them to clean their pillowcases can be a cultural shift that makes a big difference in households where sharing is the norm. Keep the tone friendly and the advice practical, and most folks bounce back without scarring.
Shubhi Sahni
23/Oct/2025Wow!!! You’ve captured the whole fungal saga so vividly, it’s like reading a thriller, with spores as sneaky villains, and antifungals as the heroic protagonists-truly a drama that unfolds on the scalp! Remember, though, that while the shampoo can wash away surface actors, the oral meds are the ones that storm the castle gates, reaching deep into the hair shaft! And don’t forget to sanitize all the “props” – combs, hats, pillows – with hot water or a bleach dip, otherwise the story might repeat itself!!!
Bonnie Lin
23/Oct/2025Consistent use of antifungal shampoo speeds up recovery.
sara fanisha
23/Oct/2025Sticking to a routine can feel tedious, but seeing new sprouts appear makes it all worth it. If you keep the scalp dry and avoid tight hats, the fungus has nowhere to hide. Small victories like fewer flakes add up to big confidence boosts.
Tristram Torres
23/Oct/2025Honestly, most people just ignore the obvious and blame dandruff, so they never get proper treatment. It’s a bit lazy to think a simple shampoo will fix a deep infection.
Abhishek Kumar
23/Oct/2025Maybe, but not everyone reads medical articles.