Osteoporosis Therapy: What Works, What Doesn't, and What to Ask Your Doctor
When you hear osteoporosis therapy, a set of medical and lifestyle approaches aimed at strengthening bones and preventing fractures in people with low bone density. Also known as bone loss treatment, it’s not just about popping a pill—it’s about understanding what’s really happening inside your bones and how to stop them from breaking. Osteoporosis isn’t just aging. It’s a silent condition where your bones slowly lose strength, often without symptoms until a fall leads to a broken hip, wrist, or spine. The good news? You can slow it down—or even reverse some of the damage—with the right plan.
Most osteoporosis therapy, a set of medical and lifestyle approaches aimed at strengthening bones and preventing fractures in people with low bone density. Also known as bone loss treatment, it’s not just about popping a pill—it’s about understanding what’s really happening inside your bones and how to stop them from breaking. starts with calcium, a mineral essential for building and maintaining strong bones, often taken as a supplement alongside vitamin D and vitamin D, a hormone-like nutrient that helps your body absorb calcium and supports muscle function to reduce fall risk. But here’s the catch: taking more calcium won’t fix everything if your body can’t use it. That’s where vitamin D comes in—without enough, calcium just passes through you. Many people over 50 are low in both, and correcting that alone can cut fracture risk by up to 30%. But if your bone density is already very low, you’ll likely need more than supplements. That’s where drugs like bisphosphonates, a class of medications that slow bone breakdown and are commonly prescribed for osteoporosis, including alendronate and risedronate come in. These aren’t magic bullets—they can cause stomach upset or rare jaw problems—but for many, they’re the difference between staying independent and ending up in a wheelchair.
Therapy isn’t just drugs and pills. It’s also about movement. Walking, lifting light weights, or doing balance exercises doesn’t just help your muscles—it tells your bones to get stronger. And it’s not just about what you do—it’s about what you avoid. Too much caffeine, smoking, or heavy drinking? They all chip away at bone health. Falls are the real danger, not the thinning bone itself. That’s why removing rugs, adding handrails, and checking your vision matter just as much as your prescription.
What you’ll find in the posts below isn’t a list of drug names. It’s real talk about what works, what doesn’t, and what people actually experience. You’ll see how timing your meds can reduce side effects, how generics compare to brand names, and why some supplements that sound helpful might not be. There’s no fluff. Just clear, practical info to help you make smarter choices with your doctor—so you don’t just survive osteoporosis, you live well despite it.
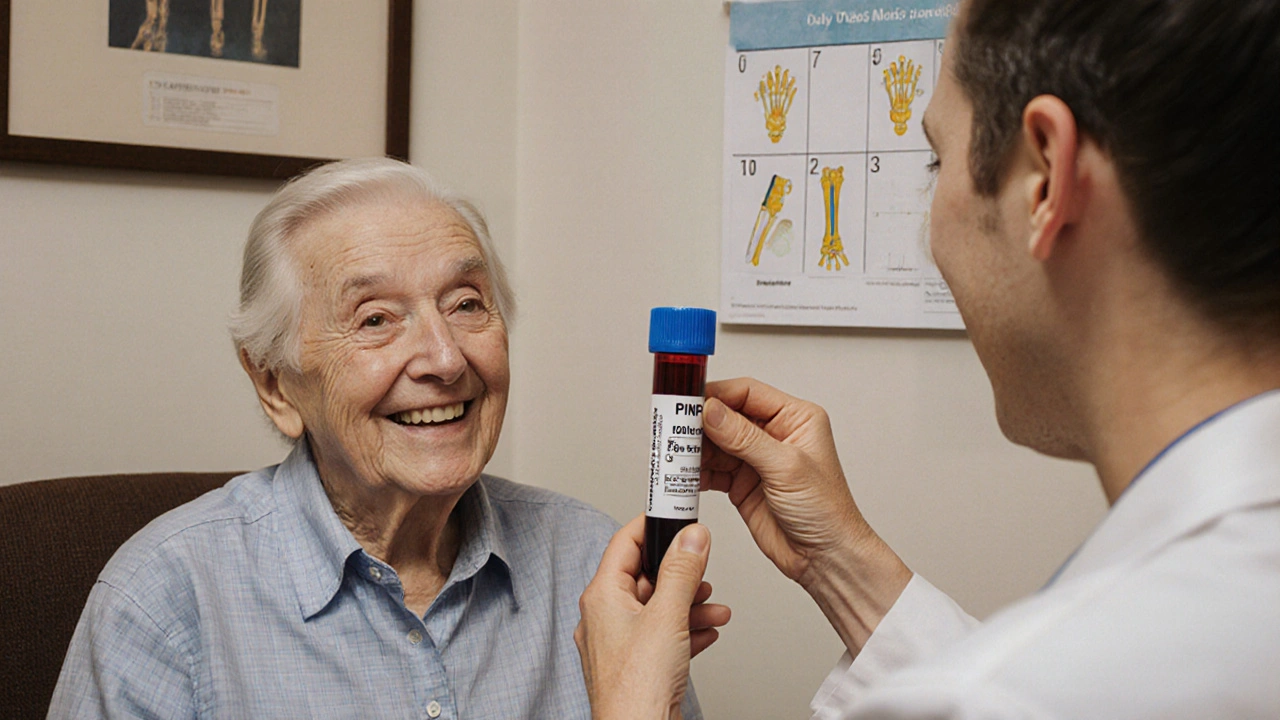
Bone Turnover Markers: How They Help Monitor Osteoporosis Treatment
Bone turnover markers like PINP and β-CTX-I offer early, reliable insight into how well osteoporosis treatments are working-within weeks, not years. Learn how they guide therapy and improve outcomes.
Read