Gluten Sensitivity
When dealing with gluten sensitivity, a condition where the body reacts negatively to gluten proteins found in wheat, barley, and rye. Also known as gluten intolerance, it can trigger digestive upset, fatigue, headaches, and skin rashes. Related conditions such as Celiac disease, an autoimmune disorder that damages the small intestine when gluten is consumed and Non‑celiac gluten sensitivity, a milder, non‑autoimmune reaction to gluten share many symptoms, but the underlying mechanisms differ. Managing the condition usually means adopting a gluten‑free diet, a nutritional plan that excludes all sources of gluten and emphasizes naturally safe foods. Understanding these connections helps you know why a strict diet is often the first line of defense.
Key aspects of gluten sensitivity
First off, symptoms are a mix of gastrointestinal and extra‑intestinal clues. Bloating, gas, and diarrhea are common, but many people also report brain fog, joint pain, or unexplained weight loss. Because these signs overlap with other disorders, a proper diagnosis is crucial. Doctors typically start with blood tests that look for antibodies linked to celiac disease; if those are negative but symptoms persist, they may recommend an elimination trial of gluten for several weeks. In some cases, an intestinal biopsy is performed to rule out celiac disease definitively. The diagnostic pathway shows that gluten sensitivity requires both clinical observation and targeted testing, linking the condition tightly to medical evaluation tools.
Once you have a clear diagnosis, the practical side kicks in. A gluten‑free diet isn’t just about reading labels; it involves learning which hidden sources—like sauces, processed meats, and even some medications—can sneak gluten into your routine. Many find it helpful to use apps or printable guides that list safe foods and common gluten traps. Nutritionists often suggest bolstering the diet with naturally gluten‑free grains such as quinoa, rice, and buckwheat, while also monitoring nutrient intake to avoid deficiencies in fiber, iron, and B vitamins. Pairing dietary changes with regular follow‑up appointments ensures you track symptom improvement and adjust the plan as needed. This blend of careful diagnosis, dietary strategy, and ongoing monitoring creates a comprehensive approach to handling gluten sensitivity.
Below you’ll find a curated collection of articles that dive deeper into each of these areas—symptom checklists, step‑by‑step testing guides, meal planning tips, and expert advice on living gluten‑free. Whether you’re just suspecting a problem or already managing the condition, the resources here will give you actionable insight to take control of your health.
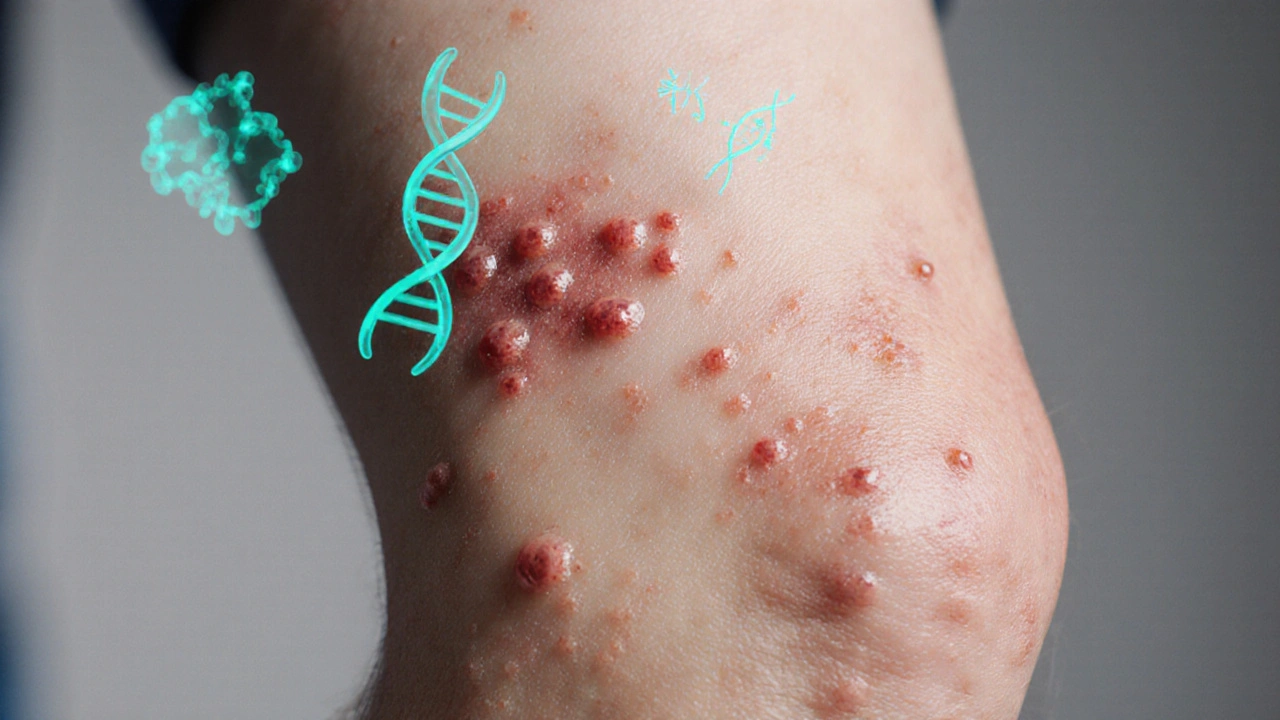
How Genetics Drive Dermatitis Herpetiformis: What You Need to Know
Explore how genetics, especially HLA-DQ2/DQ8, drive dermatitis herpetiformis, its link to celiac disease, testing, family risk, and management.
Read