What Exactly Is Nonallergic Rhinitis?
You wake up every morning with a runny nose, stuffed-up sinuses, and constant sneezing. You’ve tried antihistamines, avoided pollen, even cleaned your house top to bottom-but nothing helps. If this sounds familiar, you might have nonallergic rhinitis. Unlike allergic rhinitis, where your body overreacts to things like dust or pet dander, nonallergic rhinitis has no allergy trigger. No IgE antibodies. No positive skin tests. Just a nose that’s overly sensitive to everyday things around you.
This condition isn’t rare. About 1 in 5 adults in the U.S. and Europe deal with it. It’s more common as you get older, especially after 50. Many people spend years thinking they have allergies, only to find out their nose is reacting to something else entirely. The real problem? Most doctors still misdiagnose it. Studies show up to 40% of nonallergic rhinitis cases are wrongly treated as allergies, leading to useless medications and ongoing frustration.
The Top 6 Triggers You Can’t Ignore
Nonallergic rhinitis doesn’t care about pollen counts. It cares about what’s in the air, what you eat, and even the weather outside. Here are the six most common triggers-and the exact levels that set off symptoms.
- Environmental irritants: Tobacco smoke at just 0.05 mg/m³, perfume at 0.1 parts per million, or paint fumes above 50 ppm of VOCs can trigger a reaction. Even wildfire smoke at 15 µg/m³ of PM2.5 particles is enough.
- Weather shifts: A temperature drop or rise of more than 5°C in an hour? That’s enough. Humidity changes over 20%? Same thing. Barometric pressure shifts of just 5 mmHg can make your nose swell up.
- Food and drink: Spicy food with capsaicin (like chili peppers) at 0.5 ppm triggers runny nose in many. Alcohol? Blood alcohol levels above 0.02%-that’s less than one drink for most people-can cause nasal dripping.
- Medications: ACE inhibitors (for blood pressure) cause symptoms in 20% of users within weeks. Beta-blockers affect 15%. Even NSAIDs like ibuprofen can trigger it in 10-15% of people. Hormone replacement therapy? 8-12% of users.
- Hormonal changes: Pregnancy affects 20-30% of women, especially in the second trimester. Puberty and thyroid problems also play a role.
- Workplace exposures: Flour dust at 2 mg/m³, latex particles over 2 µg/m³, or chemical fumes at work can turn your nose into a faucet. This is called occupational rhinitis and accounts for up to 20% of work-related breathing issues.
What’s wild is that these triggers don’t cause inflammation like allergies do. Instead, they overstimulate the nerves in your nose. Think of it like a faulty thermostat-your nose thinks it’s too cold, too hot, or too dry, and responds by flooding itself with fluid.
How Doctors Diagnose It (And Why You Might Be Misdiagnosed)
If your nose is always runny, your doctor will likely test you for allergies first. That’s standard. But here’s the catch: if your skin prick test and blood test for IgE come back negative, and your symptoms last longer than 3 months, you’ve got nonallergic rhinitis. Simple as that.
Yet, studies show only 25-30% of primary care doctors correctly identify it. Most patients wait over 3 years for the right diagnosis. Why? Because the symptoms look identical to allergies: sneezing, congestion, runny nose. The only way to tell the difference is through exclusion. No allergy markers? Then it’s not allergic rhinitis.
Doctors may also use nasal endoscopy to check for polyps or structural issues, and nasal cytology to look at the cells in your mucus. In allergic rhinitis, you’ll see lots of eosinophils. In nonallergic, it’s mostly neutrophils-65-75% of the time. That’s a key clue.
First-Line Treatments That Actually Work
Forget antihistamines. They barely help here. The real solutions are simpler, cheaper, and backed by solid science.
- Nasal saline irrigation: Use a neti pot or squeeze bottle with sterile saline (0.9% isotonic or 3% hypertonic). Twice a day cuts symptoms by 60-70%. People who do this consistently report better smell, less need for sprays, and fewer sinus infections.
- Trigger avoidance: If perfume sets you off, ditch scented candles and laundry detergents. If cold air triggers you, wear a scarf over your nose in winter. If spicy food causes problems, reduce capsaicin intake. Simple changes can reduce symptoms by 25-50%.
- HEPA filters: Use one in your bedroom. They remove 99.97% of particles 0.3 microns and larger. Studies show this cuts symptoms by 35-40%.
These aren’t fancy. But they’re the foundation. Skip them, and nothing else will work as well.
Prescription Sprays That Make a Real Difference
If basic steps aren’t enough, these nasal sprays are your next move.
- Intranasal corticosteroids (like fluticasone): The gold standard. Reduces congestion and runny nose by 50-60%. Takes 2-4 weeks to peak. Side effects? Nosebleeds in 15-20% of users.
- Ipratropium bromide (Atrovent): This one’s magic for runny nose. Blocks nerve signals that cause dripping. Works in 48 hours. Reduces rhinorrhea by 70-80%. No effect on congestion. FDA-approved and safe for long-term use.
- Azelastine nasal spray: An antihistamine spray that actually works here-though only 30-40% symptom reduction. Onset is fast (1-2 hours), but the bitter taste turns off many users.
Important: Don’t use decongestant sprays like oxymetazoline (Afrin) for more than 3 days. Overuse leads to rhinitis medicamentosa-a rebound effect where your nose gets worse the more you use it. Recovery takes 7-10 days of steroid sprays and patience.
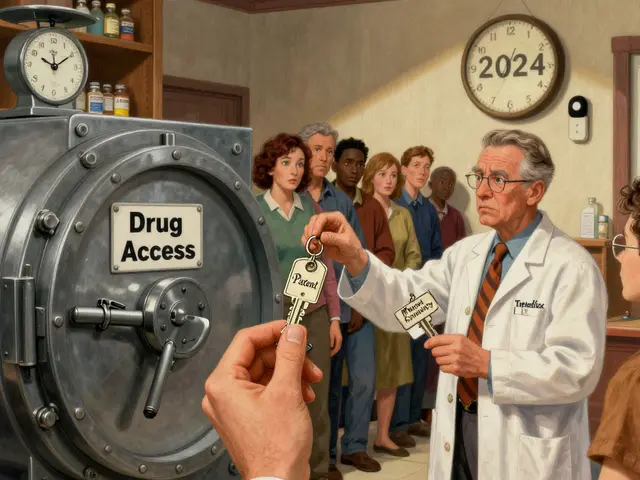
What Doesn’t Work (And Why You’re Wasting Money)
Oral antihistamines? They’re useless for nonallergic rhinitis. The American Rhinologic Society says they shouldn’t be used at all. Same with allergen immunotherapy (allergy shots). If you’ve been getting shots for years and still have a runny nose, you’ve been misdiagnosed.
Herbal remedies, steam inhalation, and essential oils? No strong evidence. Some people swear by them, but they don’t change the underlying nerve sensitivity. And they can even be irritants themselves-especially essential oils, which trigger symptoms in up to 12% of users.

What’s Coming Next: New Treatments on the Horizon
The future is looking brighter. In March 2023, the FDA approved a new, lower-dose version of ipratropium (0.03%) with fewer side effects. In September 2023, Europe accepted a new drug called BCT-100, a TRPV1 antagonist that targets the overactive nerve receptors in your nose. Early trials showed 55% symptom reduction.
Researchers are also testing tiny devices that send gentle electrical pulses through the nose to calm overactive nerves. Early results from Johns Hopkins show a 45% drop in symptoms. These aren’t available yet, but they’re coming fast.
Real People, Real Results
On patient forums, the most common success story? Ipratropium. Users on Drugs.com give it a 4.2/5 rating. Many say, “My runny nose disappeared within a day.” Saline irrigation gets 4.0/5. People say it “gave me my sense of smell back.”
But the biggest complaint? Lack of understanding. One woman wrote: “I’ve been told I’m just being dramatic. My doctor said, ‘It’s just allergies.’ I cried in the parking lot.” That’s the reality. Most people don’t know this condition exists.
Successful patients keep a symptom diary for 4-6 weeks. They track temperature, humidity, what they ate, what they smelled, and what meds they took. Then they spot patterns. “Every time I walk into the grocery store, I sneeze.” “My nose drips every time I drink wine.” That’s how they find their triggers.
Final Thoughts: You’re Not Alone
Nonallergic rhinitis isn’t dangerous. But it’s exhausting. It messes with sleep, work, and confidence. The good news? It’s manageable. You don’t need to live with a constant drip or a stuffed-up nose.
Start with saline rinses and trigger tracking. Skip the antihistamines. Talk to an ENT or allergist who knows the difference between allergic and nonallergic. And remember: you’re not imagining it. Your nose isn’t broken-it’s just hypersensitive. And that’s something you can fix.
Can nonallergic rhinitis turn into allergies?
No, nonallergic rhinitis doesn’t turn into allergic rhinitis. They’re two different conditions with different causes. But you can have both at the same time. If you develop new symptoms after exposure to pollen or pets, you might have developed an allergy on top of your existing nonallergic rhinitis. Testing can confirm this.
Is nonallergic rhinitis worse in winter?
Yes, for many people. Cold, dry air is a major trigger. Indoor heating also lowers humidity and circulates irritants like dust and chemicals. Temperature shifts between outdoors and indoors (like walking from a cold street into a warm store) can set off symptoms. Wearing a scarf over your nose helps reduce the shock to your nasal passages.
Why do spicy foods make my nose run?
Spicy foods contain capsaicin, which activates TRPV1 receptors in your nose. These are the same nerve sensors that respond to heat and irritants. When triggered, they send signals that cause your nasal glands to produce extra fluid. It’s not an allergy-it’s a direct nerve response. This is why even non-allergic people get a runny nose from hot peppers.
Can I use nasal sprays forever?
Intranasal corticosteroids and ipratropium are safe for long-term use. They don’t cause dependency. Decongestant sprays (like Afrin) are the only ones you should limit to 3 days. If you’ve been using decongestants for weeks, stop them slowly under a doctor’s guidance-rebound congestion can last weeks.
Does stress make nonallergic rhinitis worse?
Stress doesn’t cause it, but it can make symptoms feel worse. When you’re stressed, your nervous system becomes more reactive. Since nonallergic rhinitis is driven by nerve sensitivity, heightened stress can amplify your nose’s response to triggers like smells or temperature changes. Managing stress won’t cure it, but it can help you cope better.
Should I get allergy testing if I think I have nonallergic rhinitis?
Yes, absolutely. Allergy testing (skin prick or blood test) is the only way to rule out allergic rhinitis. Even if you’re sure it’s not allergies, testing confirms it. Many people have both conditions. Knowing for sure helps you choose the right treatment and avoid wasting time on ineffective meds.
For more support, check out the American Academy of Allergy, Asthma & Immunology’s patient guide or join a verified online group. You’re not alone-and better days are possible.





Comments
Edith Brederode
19/Jan/2026This is so helpful!! 🙌 I’ve been dealing with this for years and thought I was just allergic to everything. Saline rinses changed my life-my sense of smell came back after 7 years. Finally, someone gets it.
Art Gar
19/Jan/2026While the article presents itself as evidence-based, it conveniently omits the fact that the pharmaceutical industry heavily promotes nasal sprays as first-line treatments to sustain long-term revenue streams. The real solution? Reduce systemic inflammation through diet and gut health-a concept rarely discussed in conventional ENT literature.
Arlene Mathison
19/Jan/2026Y’all need to stop blaming everything on chemicals and start looking at your water! Fluoride and chlorine in tap water are wrecking nasal mucosa. I switched to filtered water and my symptoms dropped 80%. No spray needed. Why isn’t this in the article??
clifford hoang
19/Jan/2026They’re hiding the truth. The WHO and CDC know that 5G towers and EMF radiation are triggering nerve hypersensitivity in the nasal passages. That’s why it’s more common after 50-your body’s been slowly fried by decade-long exposure. The ‘TRPV1 antagonist’? Just a distraction. They don’t want you to know the real enemy is the surveillance state’s tech infrastructure. 🕵️♂️📡
Crystal August
19/Jan/2026I’m tired of people treating this like it’s just a minor annoyance. This isn’t ‘a little runny nose’-it’s a chronic, humiliating, exhausting condition that makes you feel like a broken machine. And doctors still act like you’re overreacting. It’s gaslighting with a stethoscope.
Thomas Varner
19/Jan/2026I’ve been using ipratropium for 18 months now. It works. No joke. But the bitter taste? Yeah. I mix it with a sip of cold water right after-makes it bearable. Also, I track my triggers in a Google Sheet. Turns out, my office’s air purifier emits ozone. Who knew??
Andy Thompson
19/Jan/2026America’s healthcare system is broken. You need to see a specialist to get a simple diagnosis? And insurance won’t cover saline kits unless you have a ‘code’? Meanwhile, Big Pharma pushes antihistamines like candy. This isn’t medicine-it’s a profit scheme.
Emily Leigh
19/Jan/2026So... we’re supposed to believe that a 0.02% blood alcohol level causes nasal dripping? That’s like half a beer. I drink wine every night and my nose doesn’t drip. Either this is pseudoscience or I’m somehow immune. Either way, I’m not buying it.
Shane McGriff
19/Jan/2026Hey, just wanted to say thank you to everyone sharing their stories here. I’ve been through the same thing-misdiagnosed for 4 years, felt crazy. I started the saline routine + scarf in winter, and honestly? It’s the first time in a decade I’ve slept through the night. You’re not alone. Keep tracking. Keep advocating. You’re doing better than you think.
Renee Stringer
19/Jan/2026The fact that this condition is so poorly understood speaks volumes about how medicine ignores nerve-based disorders unless they have a clear biomarker. We treat symptoms, not systems. And until we fix that, people will keep suffering in silence.