Keeping a complete and up-to-date list of all your medications isn’t just a good idea-it’s a lifesaver. Every year, around 7,000 people in the U.S. die from preventable medication errors, and many of those mistakes happen because doctors and pharmacists simply don’t know what you’re really taking. It’s not just about prescription drugs. Those vitamins, herbal supplements, or over-the-counter painkillers you grab without thinking? They matter too. A 2020 study found that proper medication reconciliation could stop 50 to 80% of errors during hospital transfers or doctor visits. That’s over a million preventable adverse events every year. This isn’t theoretical. It’s happening to real people, right now.
What Belongs on Your Medication List
Your list needs to be more than a scribble on a napkin. To be useful, it must include six key details for every medication:
- Drug name - both brand and generic (e.g., Lisinopril, not just "blood pressure pill")
- Strength/dose - 10 mg, 500 mg, etc.
- Frequency - once daily, twice a week, as needed
- Route - taken by mouth, injected, applied to skin, inhaled
- Purpose - why you take it (e.g., "for high blood pressure," "for joint pain")
- Prescribing provider - doctor’s name and clinic
Don’t forget non-prescription items. As the American Heart Association points out, many people don’t even mention supplements because they think they’re "not real medicine." But garlic pills, St. John’s wort, or even a daily aspirin can interact dangerously with blood thinners or heart medications. Also include allergies and reactions - not just "penicillin allergy," but "rash and swelling after penicillin." Exact details save lives.
Choose Your Format: Paper, App, or EHR
There’s no single best way to keep your list. The right choice depends on how you live, what tech you’re comfortable with, and your healthcare system.
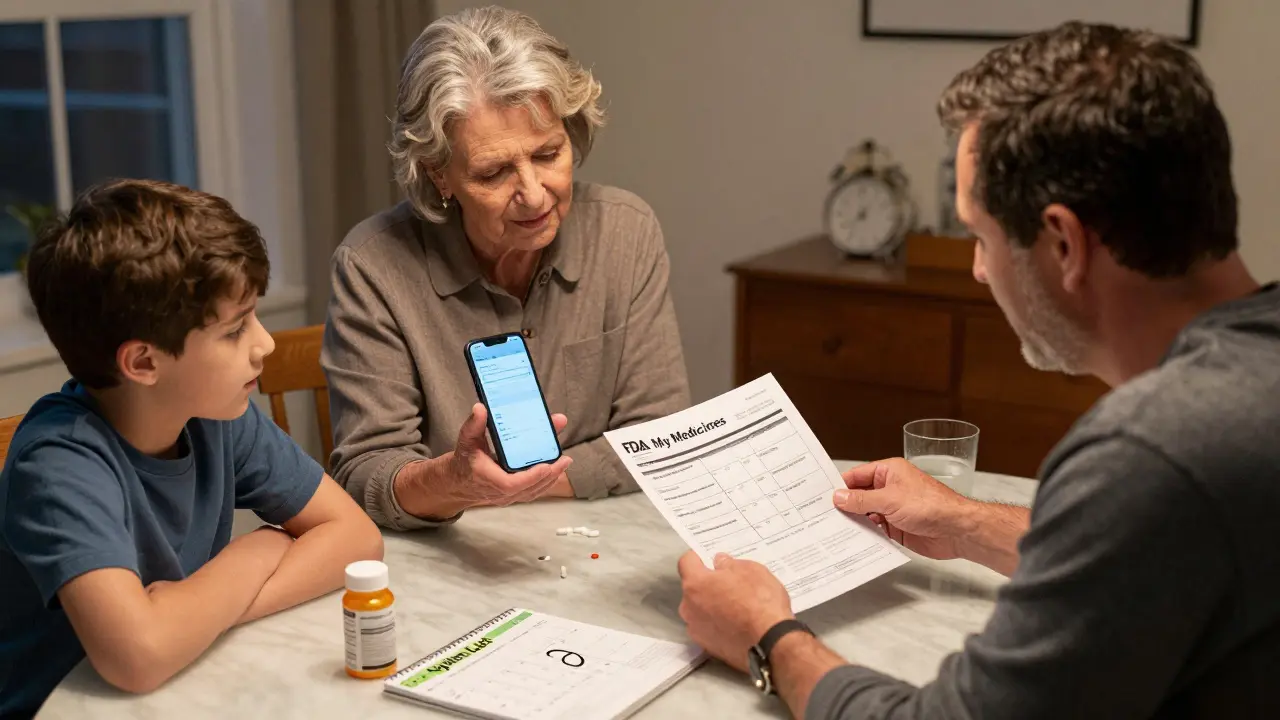
Paper lists are still widely used. The FDA’s "My Medicines" template is free, simple, and includes space for emergency contacts and allergies. The UK’s My Medication Passport works the same way. But here’s the catch: a 2022 JAMA study found that 43% of paper lists were outdated. If you use paper, update it every time you start, stop, or change a medication. Keep it in your wallet or purse - not buried in a drawer.
Smartphone apps like Medisafe, MyTherapy, and CareZone offer reminders, refill alerts, and even share lists with family or doctors. Medisafe alone is used by over 6 million people. These apps reduce missed doses by 28%, according to a 2023 BMJ Open study. But only 35% of adults over 65 use them regularly, according to Pew Research. If you struggle with screens, this might not be your fit. Some users complain about clunky interfaces - 78% of 1-star reviews mention difficulty navigating.
EHR-integrated lists (like Epic’s MyChart or Cerner’s patient portals) are becoming more common. These lists update automatically when your doctor prescribes something new. They’re accurate and accessible during appointments. But you can’t edit them yourself, and they only work if your provider uses the same system. Only 62% of U.S. hospitals have full reconciliation workflows, and just 58% of primary care offices do.
How to Build and Update Your List
Start by gathering everything. Go through your medicine cabinet, purse, and bathroom. Pull out every pill bottle, patch, inhaler, and supplement container. Write down each one using the six details above. Include things you take "as needed," like ibuprofen or antacids. Don’t forget eye drops, creams, or injections.
Then, call your pharmacy. Most can print out a complete list of everything they’ve dispensed for you in the last year. Compare it to your own list. You’ll likely find gaps - maybe a discontinued drug you forgot about, or a new one you didn’t record.
Update your list after every change. That means:
- After a hospital stay
- After seeing a new specialist
- When a prescription is refilled or changed
- When you start or stop a supplement
A 2021 University of Michigan study found 68% of patients didn’t update their list after leaving the hospital. That’s dangerous. A drug you stopped in the hospital might still be on your list - and your doctor might prescribe it again.

Use the Brown Bag Method
One of the most effective ways to keep your list accurate is to bring your actual medications to every doctor’s appointment. This is called the "brown bag method." Pack everything you take - pills, liquids, patches, inhalers - in a brown paper bag. Let your doctor or pharmacist look at them. They’ll spot duplicates, expired meds, or interactions you didn’t know about.
Geriatric pharmacists recommend this method to 82% of older patients. It’s especially helpful if you see multiple doctors or get prescriptions from different pharmacies. You don’t need to remember everything. You just need to show them the bottles.
Make Updating Part of Your Routine
People forget to update lists because it feels like a chore. Make it automatic. Pick a time that’s already part of your week - like Sunday night when you organize your pill box. Or when you refill your prescriptions. Set a phone reminder: "Update medication list every 30 days." Another trick: take a photo of each pill bottle with your phone. Store them in a folder labeled "Medications." When you’re unsure what you’re taking, just pull up the photo. No need to write anything down - just show the picture to your provider.
Why This Matters: Real Stories
A nurse in New York told Reddit users she caught three potentially fatal drug interactions in one month just by checking patients’ lists. One patient was on warfarin and had started taking a new herbal supplement. The supplement increased bleeding risk. Without the list, the doctor would’ve never known.
Kaiser Permanente cut medication-related readmissions by 22% in 18 months by training staff to always check and update medication lists before discharge. That’s thousands of people avoiding another hospital stay.
But there’s also a dark side. The ECRI Institute reported a case where an outdated list led to a fatal warfarin interaction. The patient had stopped a medication, but the list still had it. A new doctor prescribed a drug that clashed with the old one. The patient didn’t survive.
What to Do If You’re Overwhelmed
If you take five or more medications - what’s called "polypharmacy" - you’re at higher risk. The National Council on Aging found that 76% of people on five or more drugs keep a list, compared to just 32% of those on one or two. That’s because they’ve felt the danger firsthand.
Ask your pharmacist for a free Medication Therapy Management (MTM) session. Since 2011, Medicare Part D covers this service. A pharmacist will review your entire list, spot duplicates, check for interactions, and help you simplify your regimen. Many people reduce their pill count by 30% after an MTM session.
Also, ask your doctor about synchronized refills. Instead of getting 30-day refills for each drug on different dates, ask if you can get 90-day supplies with all refills due on the same day. The American Medical Association says this saves an average of 2.7 hours per physician daily - and makes it easier for you to stay on track.
Final Checklist
Here’s what you need to do right now:
- Collect all your medications - prescriptions, OTC, vitamins, supplements.
- Write down the six key details for each one.
- Call your pharmacy for a printed list to compare.
- Choose your format: paper, app, or EHR portal.
- Update the list today - and set a monthly reminder.
- Bring your brown bag to your next appointment.
You don’t need to be perfect. You just need to be consistent. Even a simple, mostly accurate list is better than no list at all. In a system where doctors often don’t know what you’re taking, your list is your voice. Use it.
Do I really need to include over-the-counter drugs and supplements?
Yes. Many dangerous interactions happen because of OTC drugs and supplements. For example, St. John’s wort can make birth control, antidepressants, or blood thinners ineffective. Ibuprofen can raise blood pressure or damage kidneys when taken with certain heart medications. Even a daily aspirin or vitamin E can interfere with surgery or other treatments. If you take it, it belongs on the list.
What if I forget to update my list after a change?
Don’t panic - but don’t wait. The biggest risk isn’t forgetting once - it’s letting outdated information stay in your records. If you realize you missed an update, correct it as soon as possible. Bring your updated list to your next appointment. If you’re seeing a new doctor, tell them: "I recently changed my meds - here’s what’s current." Most providers will ask for a list, so they’ll expect this.
Can I trust my pharmacy’s list?
Pharmacy lists are usually accurate for prescriptions they’ve filled - but they won’t include supplements, vitamins, or drugs from other pharmacies. If you get prescriptions from multiple pharmacies, your list from one pharmacy won’t show everything. Always cross-check with your own records and the brown bag method.
Is there a free template I can use?
Yes. The U.S. Food and Drug Administration offers a free "My Medicines" printable template that includes space for all medications, allergies, and emergency contacts. You can find it on the FDA’s website by searching "My Medicines template." Many pharmacies also have their own versions - ask your pharmacist.
I’m on Medicare. Can I get help with my medication list?
Yes. Medicare Part D covers a free service called Medication Therapy Management (MTM). A pharmacist will review all your medications - including supplements - check for interactions, simplify your regimen, and help you understand what you’re taking. You qualify if you have multiple chronic conditions and take several medications. Ask your pharmacy or call 1-800-MEDICARE.






Comments
Autumn Frankart
13/Feb/2026I've been keeping a list for years, but last month my doctor refused to look at it because it was 'too detailed.' Said I was 'overloading the system.' Meanwhile, my meds were switched out without warning and I ended up in the ER. Coincidence? I think not. They don't want you to know what you're on. They want you dependent. I'm not just talking about pills. I'm talking about control.
They track everything. Your phone. Your Google searches. Your pharmacy records. Why wouldn't they scrub your list? I've started handwriting mine in invisible ink. Literally. Lemon juice. Dries clear. Only shows under UV light. My pharmacist thinks I'm nuts. Good. Let him be confused while I stay alive.
Skilken Awe
13/Feb/2026Let me guess - you're also one of those people who thinks 'Medication Therapy Management' is just a fancy term for 'pharmacist playing therapist while billing Medicare.'
Here's the real issue: the entire system is built on obfuscation. EHRs? Proprietary black boxes. Pharmacy logs? Fragmented across 7 different vendors. Your 'brown bag'? A performative ritual that makes doctors feel like they're doing their job without actually changing anything.
And don't get me started on 'MyChart.' I had a patient who was on warfarin, and his portal said 'aspirin 81mg daily.' Turns out he'd been on 325mg for 11 years. Portal was wrong. Nurse didn't catch it. He bled out in the waiting room. Systemic failure. Not user error.
andres az
13/Feb/2026I read the whole thing. Took me 47 minutes. Here's my takeaway: you're telling people to do more paperwork to fix a system that was designed to make paperwork inevitable.
It's like handing someone a flashlight and saying 'you're responsible for the power grid outage.'
The real solution? Ban polypharmacy. Ban supplements. Ban OTCs. Let doctors prescribe ONE thing. One. And if you need more, you go to a committee. A real one. With lawyers. And cameras. Because right now? It's chaos. And chaos is profitable.
Steve DESTIVELLE
13/Feb/2026The medication list is not a tool. It is a symptom. A symptom of a deeper fracture - the fracture between the self and the system. You are told to list your pills. But who listed the pills that made you take them? Who listed the fear that made you believe you needed them in the first place?
We live in an age of pharmacological self-optimization. We are not patients. We are data points. We are compliance metrics. We are billing codes with pulse.
The brown bag? It is not about safety. It is about surrender. You bring your pills not to be saved - but to be judged. To be told you are not doing enough. Not taking enough. Not knowing enough.
True healing begins when you stop listing your drugs - and start questioning why you were given them.
Stephon Devereux
13/Feb/2026This post is gold. Seriously. I work in geriatrics and I see this every single day. One woman came in with 23 different meds. Turned out 9 were duplicates. 4 were expired. 2 were for conditions she didn’t even have anymore. She was confused, dizzy, falling - and no one had ever sat down with her and asked: 'What are you actually taking?'
Simple fix? Start with the brown bag. Bring it. Every time. No excuses. It’s not about being perfect - it’s about being present. I’ve seen patients go from nearly comatose to sharp as a tack in 2 weeks after we cleaned up their list.
And yes - include the turmeric pills. The melatonin. The fish oil. That’s not 'alternative medicine.' That’s pharmacology. Your body doesn’t care if it’s FDA-approved. It reacts. Period.
Neha Motiwala
13/Feb/2026I tried the app. I really did. Medisafe. Then MyTherapy. Then CareZone. I set reminders. I synced with my husband. I even printed out the QR code. Then my phone died. For 3 days. And guess what? My pills were still in the bottle. But the app? It said I missed 17 doses. 17. I didn't miss any. I just didn't have electricity. So now I use paper. Handwritten. In red ink. Because if I can't trust technology to remember my meds - why should I trust it to remember my life?
athmaja biju
13/Feb/2026In India, we do not have such luxury. My father takes 11 medications. We have no EHR. No pharmacy portal. No app. We write on a torn page of a notebook. Sometimes we forget to write. Sometimes we lose the page. Sometimes the doctor doesn't read it. But we keep trying. Because if we don't, who will? This isn't about convenience. It's about survival. And survival doesn't come with a UI.
Craig Staszak
13/Feb/2026I love how this post doesn't just say 'make a list' - it gives you the why. The stats. The real stories. That's what makes it stick. I used to think this was just for elderly people. Then my mom had a stroke. She was on 8 drugs. The hospital had no idea what she was taking. We had to scramble. That's when I made our list. Now I update it every Sunday. No big deal. Just part of the routine. Like brushing teeth. Only this one saves lives.
Reggie McIntyre
13/Feb/2026I just started using the FDA template. Took me 12 minutes. I even took photos of every bottle and labeled them 'A1, A2, B1' so I can match them later. I didn't realize how many things I was taking 'as needed' - like that one antacid I took 3x a day. Whoops. Also found a 2-year-old bottle of prednisone I forgot about. Scary. But now I'm in control. I feel like a superhero. My doctor even smiled. Can you believe that? A doctor SMILED at me. For being organized. It's a new world.
Jack Havard
13/Feb/2026You're telling people to trust paper, apps, and portals - all while ignoring the fact that 80% of EHRs are built on 1990s code. And the apps? They sell your data. The FDA template? It's a marketing tool. The 'brown bag'? A circus act. They want you to feel responsible. So they don't have to fix the system.
I don't make lists. I make noise. I call my pharmacy. I call my doctor. I call my insurance. I scream until someone listens. That's how you survive. Not by writing down pills. By breaking the system.
Gloria Ricky
13/Feb/2026I just updated mine! I forgot about my ginkgo biloba and my magnesium - and I take them every single night! I’m so glad I read this. I was gonna skip my next appt bc I was tired. But now I’m gonna bring my bag. I even wrote ‘DO NOT PRESCRIBE BLOOD THINNER’ in big letters on the top. My pharmacist said I’m a legend. I cried a little. Not because I’m sad. Because I finally feel like I’m not alone.
Stacie Willhite
13/Feb/2026I used to think this was just for older people. Then my sister had a bad reaction to a new antibiotic. Turned out she’d been taking St. John’s wort for anxiety. No one asked. No one checked. She almost didn’t make it.
Now I help my friends make their lists. I don’t judge. I don’t push. I just sit with them. We go through the cabinet. We laugh. We cry. We remember. It’s not about the paper. It’s about the care. And that’s worth more than any app.
Jason Pascoe
13/Feb/2026I'm from Australia. We don't have the same system. My GP has my full record. My pharmacy has my full record. My specialist has my full record. They all talk. I don't need a list. But I still bring my brown bag. Why? Because it's a conversation starter. And sometimes, the best medicine isn't in the pill - it's in the question you didn't know to ask.