DPP-4 Inhibitor Joint Pain Checker
Assess Your Joint Pain
Answer these questions to determine if your joint pain might be related to DPP-4 inhibitors (Januvia, Onglyza, Tradjenta). This tool is for informational purposes only and does not replace medical advice.
If you’re taking a DPP-4 inhibitor for type 2 diabetes, and your knees, hips, or hands have started hurting out of nowhere, you’re not imagining it. This isn’t just aging or overuse - it could be a known, but often missed, side effect of your medication. The FDA first sounded the alarm in 2015, and since then, thousands of patients have reported sudden, severe joint pain linked to drugs like sitagliptin (Januvia), saxagliptin (Onglyza), and linagliptin (Tradjenta). Most doctors don’t mention it during the initial consultation. But if you’re experiencing unexplained, persistent joint pain, this is something you need to know.
What Are DPP-4 Inhibitors?
DPP-4 inhibitors are oral diabetes medications that help control blood sugar by boosting natural hormones that tell your body to release insulin after meals. They’re often prescribed when metformin alone isn’t enough, or when patients can’t tolerate other drugs. The most common ones are sitagliptin, saxagliptin, linagliptin, and alogliptin. Vildagliptin is used outside the U.S. These drugs don’t cause weight gain or low blood sugar on their own - which is why they’re popular. But they’re not harmless.
The Joint Pain Connection
The FDA reviewed over 7 years of adverse event reports and found 33 clear cases of severe, disabling joint pain directly tied to DPP-4 inhibitors. That might sound rare - and it is - but the pattern is unmistakable. In 22 of those cases, pain started within just one month of starting the drug. In others, it took up to a year. The pain wasn’t mild. Patients couldn’t walk, couldn’t work, and 10 needed hospitalization. One woman developed intense knee pain three weeks after starting sitagliptin. Her pain vanished two weeks after stopping it - and came right back when she accidentally took it again.
This isn’t just anecdotal. A 2021 study using real-world data from over 250 million Americans found that people on DPP-4 inhibitors were 24% more likely to seek medical care for joint pain than those on other diabetes drugs. Another study of older veterans showed a 17% higher risk. Even though most patients don’t get severe pain, the risk is real enough that the FDA requires warning labels on all these drugs.
How Bad Is the Pain?
Patients describe it as deep, aching, and symmetrical - meaning both sides of the body hurt at once. Knees and hands are most common, but hips, shoulders, and even the spine can be affected. It’s not like arthritis that flares up after activity. This pain often hits at rest, wakes you up at night, and doesn’t improve with rest or over-the-counter painkillers. Many patients are misdiagnosed with rheumatoid arthritis, lupus, or gout. One man spent months seeing rheumatologists before his doctor finally asked: “When did you start your diabetes pill?”

Why Does This Happen?
No one knows for sure. DPP-4 isn’t just in the pancreas - it’s in joints, skin, and immune cells. Some researchers think blocking it might trigger inflammation in joint tissues. Others suspect it affects immune signaling in ways we don’t fully understand. What we do know: when patients stop the drug, pain usually fades within days to weeks. In 23 out of 33 FDA cases, symptoms disappeared within a month. And when people took the same drug again, the pain returned - a classic sign of a drug reaction.
What Should You Do?
Don’t stop your medication on your own. These drugs help prevent heart attacks, kidney damage, and nerve problems in people with diabetes. But if you’re having new, unexplained joint pain - especially if it’s severe or worsening - talk to your doctor. Tell them exactly when it started, how bad it is, and whether it’s affecting your daily life. Bring up the FDA warning. Ask: “Could this be from my DPP-4 inhibitor?”
Your doctor may suggest switching to another diabetes drug - like an SGLT2 inhibitor or GLP-1 receptor agonist - that doesn’t carry this risk. In most cases, pain resolves completely after stopping the drug. If you’ve been on it for years and just started feeling pain, don’t assume it’s “just getting older.” That delay in diagnosis is exactly why this side effect is so dangerous.
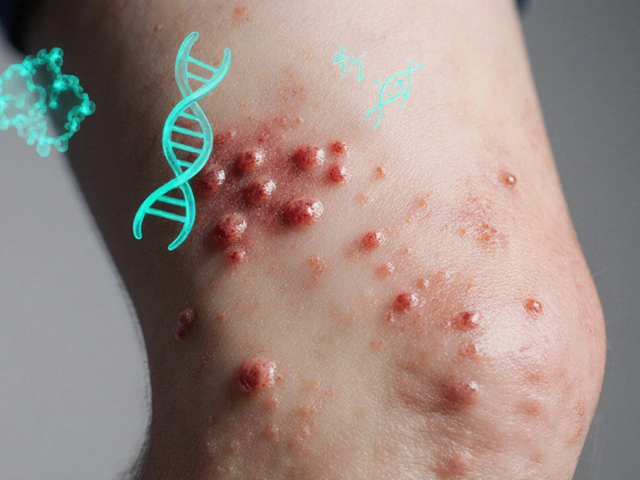
Other Side Effects to Watch For
Joint pain isn’t the only risk. DPP-4 inhibitors have also been linked to pancreatitis - inflammation of the pancreas - which can be life-threatening. Some patients develop serious skin reactions like bullous pemphigoid, where blisters form on the skin and mucous membranes. Rarely, there are allergic reactions, including swelling of the face or throat. If you notice blisters, swelling, or sudden breathing trouble, seek emergency care.
For most people, these side effects never happen. But if you’re one of the few who do experience them, catching it early makes all the difference.

What the Experts Say
The American Diabetes Association acknowledges the risk but says the overall chance of severe joint pain is low - especially compared to the benefits of controlling blood sugar. Johns Hopkins and the Cleveland Clinic both advise doctors to consider DPP-4 inhibitors as a possible cause of new joint pain in diabetic patients. The European Medicines Agency issued a similar warning in 2015, and follow-up data from 2023 still reminds clinicians: “Don’t overlook this.”
Doctors aren’t ignoring it anymore. More are asking patients about joint pain during routine check-ups. But you can’t wait for them to ask. If you’re on one of these drugs and your body feels off, speak up.
What If You’ve Already Stopped?
If you stopped your DPP-4 inhibitor because of joint pain and felt better - good. Keep track of how long it took to improve. If you ever need to restart diabetes medication, tell your doctor what happened. There are plenty of other options. SGLT2 inhibitors like empagliflozin (Jardiance) and GLP-1 drugs like semaglutide (Ozempic) are now first-line choices for many patients, especially those with heart or kidney risks. They don’t cause joint pain.
Even if you’ve been on a DPP-4 inhibitor for years without issues, don’t assume you’re immune. The pain can start anytime - even after 12 months. That’s why ongoing awareness matters.
Final Thoughts
DPP-4 inhibitors work well for millions. But for a small number, they cause pain that turns lives upside down. If you’re on one of these drugs and your joints are hurting, don’t brush it off. Don’t wait for your doctor to notice. Document your symptoms. Note when they started. Track how they change. Bring this to your next appointment. You might be the one who helps your doctor catch something others miss.
Diabetes management is about balance. You want to protect your heart, kidneys, and nerves - but you also need to protect your mobility, your independence, your quality of life. If your medication is stealing that, it’s time to talk about alternatives.




Comments
Ian Cheung
8/Jan/2026Man I thought my knees were just failing me from all that weekend hiking turns out it was Januvia. I stopped it cold turkey and within 10 days the pain was gone like it never existed. My doctor acted like it was my imagination until I showed him the FDA warning. Now he asks every patient on DPP-4s about joint pain. Seriously if you're hurting and on one of these meds don't wait like I did
Saumya Roy Chaudhuri
8/Jan/2026OH MY GOD THIS IS WHY I COULDN'T WALK FOR THREE MONTHS!! I WAS TOLD IT WAS 'OLD AGE' AND 'OSTEOARTHRITIS' UNTIL I FINALLY ASKED ABOUT MY MEDS. THEY WERE GIVING ME PAINKILLERS AND STEROIDS WHEN ALL I NEEDED WAS TO STOP THE DRUG. I'M SO ANGRY I LOST SO MUCH TIME. THIS NEEDS TO BE ON EVERY PRESCRIPTION LABEL IN BOLD RED
anthony martinez
8/Jan/2026Interesting that the FDA found 33 cases. That’s less than 0.001% of users. Meanwhile, thousands die every year from uncontrolled diabetes. I’m not saying it doesn’t happen, but let’s not turn a rare side effect into a panic.
Mario Bros
8/Jan/2026Bro this is real. My mom was on saxagliptin for 14 months and suddenly couldn't climb stairs. She thought she was getting old. We switched her to Jardiance and boom - two weeks later she’s gardening again. Don’t ignore it. Your body’s screaming. Listen.
Christine Milne
8/Jan/2026It is regrettably evident that the proliferation of anecdotal evidence, unsupported by statistically significant longitudinal studies, has precipitated a public health misdirection. The American Medical Association has not issued any formal advisory, and the FDA’s warning, while technically accurate, is disproportionately amplified by social media hysteria. One must not conflate temporal association with causation.
Michael Marchio
8/Jan/2026Look, I’ve been prescribing these for over a decade. Most patients are fine. But I’ve had three patients in the last year come in with joint pain that vanished the moment they stopped the drug. And then it came back when they were restarted. That’s not coincidence. That’s pharmacology. The problem isn’t the drug - it’s that doctors don’t ask the right questions. Patients don’t connect the dots. And by the time they do, they’ve already lost months of mobility. It’s not the drug’s fault. It’s the system’s.
neeraj maor
8/Jan/2026Did you know DPP-4 inhibitors were originally developed by pharmaceutical companies that also manufactured NSAIDs? The joint pain side effect? It’s not a side effect - it’s a business model. Keep people on painkillers while they’re on the diabetes drug. More profit. The FDA is a revolving door. The same people who approved these drugs now sit on advisory boards for the manufacturers. Wake up.
Ritwik Bose
8/Jan/2026Thank you for sharing this important information 🙏. I have a patient from Delhi who experienced similar symptoms - she stopped her medication and within 12 days, her hand pain resolved completely. I now routinely screen for joint discomfort in all patients on DPP-4 inhibitors. Small changes in clinical practice can prevent immense suffering. Let us remain vigilant, compassionate, and evidence-based.
Aurora Memo
8/Jan/2026I’m glad this is getting attention. My sister was misdiagnosed for months. She thought she had rheumatoid arthritis. It wasn’t until she mentioned her new diabetes pill that her doctor connected the dots. She’s fine now, but the anxiety and pain she went through? Unnecessary. If you’re on one of these, pay attention to your body. And if you’re a doctor - ask the question. Even if it seems obvious.
chandra tan
8/Jan/2026In India, we call this 'medicine sickness' - when the cure starts hurting more than the disease. My uncle was on Januvia for two years, then suddenly couldn't hold his chai cup. He thought it was arthritis. We switched him to metformin and now he plays cricket with his grandkids again. Don't trust the hype, but don't ignore your body either. Talk to your doctor. Simple.