When you’re prescribed a new medication, you might hear your doctor or pharmacist mention a biosimilar or a generic. Both sound like cheaper versions of brand-name drugs, but they’re not the same. Choosing the wrong one-or misunderstanding the difference-can lead to confusion, anxiety, or even delays in treatment. If you’re managing a chronic condition like rheumatoid arthritis, diabetes, or cancer, knowing whether you’re getting a biosimilar or a generic isn’t just about saving money. It’s about safety, effectiveness, and peace of mind.
What’s the Real Difference Between Generics and Biosimilars?
Generics are exact chemical copies of brand-name drugs. Think of them like photocopies: same ink, same paper, same words. If your doctor prescribes Lipitor for cholesterol, the generic version, atorvastatin, contains the exact same molecule. It works the same way, in the same dose, with the same side effects. The FDA requires generics to prove they’re bioequivalent-meaning your body absorbs and uses them identically to the brand-name drug. That’s why you can swap them at the pharmacy without telling your doctor.
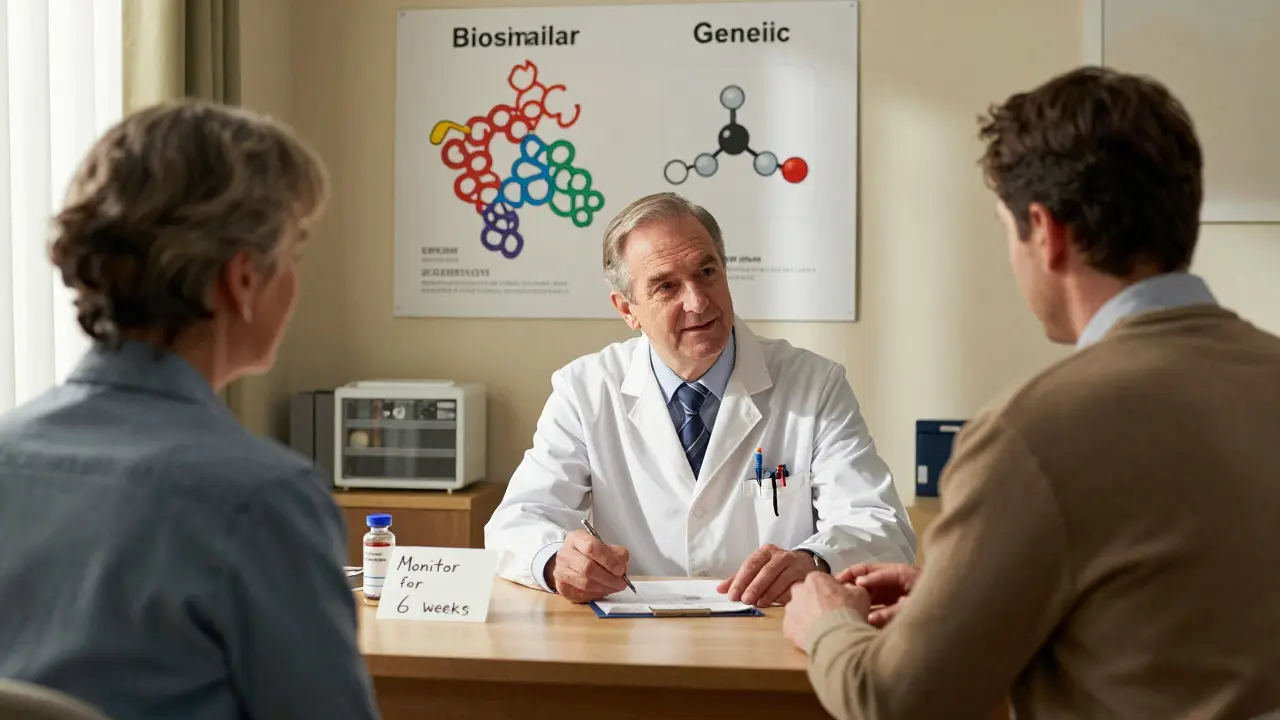
Biosimilars are different. They’re not copies. They’re highly similar versions of biologic drugs-medicines made from living cells, like proteins or antibodies. Drugs like Humira (adalimumab), Enbrel (etanercept), or Herceptin (trastuzumab) are made in bioreactors using living organisms, not chemical labs. Even tiny changes in temperature, pH, or cell line during production can alter the final product. That’s why biosimilars can’t be identical. The FDA calls them “highly similar,” meaning they match the original in structure, function, safety, and effectiveness-with no clinically meaningful differences.
Here’s a simple way to remember: Generics = identical chemical molecules. Biosimilars = nearly identical large proteins made by living cells.
Why Cost Savings Are Very Different
Generics save you a lot. On average, they cost 80-85% less than the brand-name drug. A 30-day supply of brand-name Lipitor might be $150. The generic? Around $10-$20. That’s why generics make up over 90% of all prescriptions filled in the U.S.
Biosimilars don’t save as much-typically 15-20% off the price of the original biologic. Why? Because making them is incredibly expensive. While a generic drug costs $2-$3 million to develop, a biosimilar can cost $100-$250 million. That’s because scientists must use advanced tools like mass spectrometry and chromatography to prove the molecule behaves the same way. They also need to run clinical trials, even if they’re smaller than those for the original drug.
So if you’re on a biologic that costs $20,000 a year, switching to a biosimilar might cut your bill to $16,000-not $4,000. Still, that’s $4,000 saved annually. For many patients, that’s life-changing.
When Can You Switch? The Rules Are Not the Same
With generics, switching is easy. In 49 U.S. states, pharmacists can substitute a generic for a brand-name drug automatically-unless your doctor writes “dispense as written.” No notice. No paperwork. Just a cheaper pill.
Biosimilars? It’s more complicated. Only “interchangeable” biosimilars can be swapped at the pharmacy without the prescriber’s approval. As of 2025, only a handful have received this designation from the FDA-like Semglee (insulin glargine) and Cyltezo (adalimumab). Even then, 28 states require the pharmacist to notify your doctor within 72 hours of the switch. Some insurers require prior authorization. Some doctors still hesitate to allow it.
That’s why many patients don’t even know they’ve been switched. A 2023 study found only 35% of eligible patients received a biosimilar prescription, even when it was cheaper and approved. Why? Many prescribers aren’t trained to explain the difference. Patients hear “new drug” and worry.
Are They Safe? The Evidence Says Yes
Let’s be clear: both generics and biosimilars are rigorously tested. The FDA doesn’t approve them just because they’re cheaper. They have to prove they work the same way.
For generics, over 47 clinical trials reviewed by JAMA in 2019 showed no difference in effectiveness between brand-name and generic heart medications. The same goes for epilepsy, depression, and blood pressure drugs.
For biosimilars, the data is just as strong. A 2022 review of 128 studies involving over 38,000 patients found no meaningful difference in safety or effectiveness between the reference infliximab (Remicade) and its biosimilar. Real-world data from cancer centers shows patients on biosimilar trastuzumab (Herceptin) have the same tumor response rates as those on the original.
One concern is immunogenicity-whether the body might react to the biosimilar as if it’s foreign. That’s a valid question. But the FDA’s adverse event database shows biosimilars have a safety profile nearly identical to the original. For example, biosimilar infliximab had 0.12 adverse events per 100 patient-years; the original had 0.15. The difference wasn’t statistically meaningful.
Still, some patients report anxiety after switching. One patient on a rheumatoid arthritis forum wrote, “I was scared. I thought my joints would flare.” But after three months, her pain scores didn’t change. She saved $8,000 a year.
What About Storage and Handling?
This is something most people don’t think about-but it matters.
Generics are usually stable at room temperature. You can leave them in your medicine cabinet. No special handling needed.
Biosimilars? Most require refrigeration (2-8°C). If they’re exposed to heat, they can break down. That’s why delivery, storage, and even how your pharmacy handles them matters. A 2023 study found that 12% of biosimilar errors in clinics were due to temperature mishandling-like leaving a vial on a counter during a busy shift.
Patients on insulin biosimilars like Basaglar sometimes report trouble with the pen device. It looks different from Lantus. One Reddit user wrote: “I accidentally set the dose wrong because the dial felt different. I didn’t realize it wasn’t the same pen.”
If you’re switching to a biosimilar, ask your pharmacist: “Will this need special storage? Is the delivery device the same?”

Who Decides? Your Doctor, Your Pharmacist, Your Insurance
It’s not just about what’s available. It’s about who controls access.
Insurance companies often push for biosimilars because they’re cheaper than the original biologic. But they might not cover them unless you’ve tried the brand-name first. That’s called “step therapy.”
Doctors vary too. A 2023 AMA survey found only 58% of non-specialist physicians felt “very confident” prescribing biosimilars. Specialists-like oncologists and rheumatologists-are more familiar with them. That’s why your experience might depend on who you see.
Support programs help. Companies like Amgen and Pfizer offer patient assistance for their biosimilars: free education, financial aid, even nurse hotlines. These don’t exist for generics.
What Should You Do?
Here’s a simple guide:
- Know what you’re on. Is it a small-molecule drug (like metformin, lisinopril, or atorvastatin)? Then it likely has a generic. Ask if you can switch.
- Is it a biologic? (Like Humira, Enbrel, Herceptin, or insulin)? Then you’re looking at a biosimilar, not a generic. Generics don’t exist for these.
- Ask your doctor: “Is there a biosimilar or generic option for this?” Don’t assume they know.
- Ask your pharmacist: “Is this a biosimilar? Is it interchangeable? Does it need refrigeration?”
- Check your insurance. Do they require prior authorization? Do they cover the biosimilar at a lower copay?
- Don’t panic if you’re switched. If you’re moved to a biosimilar and feel fine after 6-8 weeks, you’re likely doing great.
What’s Coming Next?
The biosimilar market is exploding. In 2023, it was worth $12.4 billion. By 2030, it’s projected to hit $58.7 billion. New biosimilars for Stelara (ustekinumab), Keytruda, and Rituxan are coming soon. These could save patients billions.
The Inflation Reduction Act of 2022 helped too. Medicare providers now get full reimbursement for biosimilars-no penalty. That’s speeding up adoption.
But the biggest barrier isn’t science. It’s awareness. Many patients still think “biosimilar = less effective.” That’s not true. The science says otherwise.
What you need to know: Biosimilars aren’t the same as generics. But they’re both safe, effective, and regulated. The goal isn’t to pick one over the other-it’s to use the right tool for the right drug. And if you can save money without risking your health? That’s a win.
Are biosimilars as safe as brand-name biologics?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original biologic. Real-world data from over 38,000 patients shows no increase in side effects or treatment failure. Adverse event rates are nearly identical.
Can I switch from a brand-name drug to a biosimilar on my own?
No. Only pharmacists can switch you to an “interchangeable” biosimilar-and even then, only if your state allows it and your doctor hasn’t blocked substitution. Never switch without talking to your prescriber first. Some conditions, like cancer or autoimmune diseases, require close monitoring after any change.
Why are biosimilars more expensive than generics?
Because they’re made from living cells, not chemicals. Producing a protein drug requires complex bioreactors, strict temperature controls, and advanced testing to prove it’s highly similar to the original. Development costs range from $100-$250 million, compared to $2-$3 million for generics.
Do I need to get blood tests after switching to a biosimilar?
Not routinely. For most patients, no extra monitoring is needed. But if you have a condition like inflammatory bowel disease or rheumatoid arthritis, your doctor may check disease markers (like CRP or ESR) 6-8 weeks after switching to confirm stability. This isn’t because biosimilars are riskier-it’s just good practice when any treatment changes.
Can I get a biosimilar if I’ve never taken the brand-name drug before?
Yes. Biosimilars are approved as first-line treatments, not just switches. For example, many rheumatologists now start patients with adalimumab biosimilars instead of Humira. Insurance often prefers it too, because it’s cheaper.
Why don’t all pharmacies stock biosimilars?
Some smaller pharmacies don’t carry them due to storage requirements (refrigeration), limited demand, or complex ordering systems. Hospital pharmacies and large retail chains are more likely to stock them. If yours doesn’t, ask if they can order it-or if your doctor can prescribe it through a specialty pharmacy.





Comments
Mussin Machhour
24/Dec/2025Just switched to a biosimilar for my RA last year and saved nearly $9K. My joints didn’t flare, my insurance was thrilled, and I didn’t even notice the difference. If you’re scared, talk to your doc - but don’t let fear cost you money you could use for something life-changing.
Winni Victor
24/Dec/2025Oh great, so now Big Pharma’s gonna slip us ‘almost-the-same’ drugs and call it progress? Next they’ll say aspirin and ibuprofen are ‘biosimilar’ because both hurt your stomach the same way. 🙄
Lindsay Hensel
24/Dec/2025Thank you for this clear, compassionate breakdown. Many patients live in fear of change - especially when their health is at stake. Education, not suspicion, is the path forward.
Gary Hartung
24/Dec/2025Let’s be honest - biosimilars are a corporate ploy. The FDA? A rubber stamp. The clinical trials? Underpowered. And don’t get me started on the ‘interchangeable’ label - it’s just marketing with a lab coat.
Meanwhile, real science? Still waiting for Phase IV data that doesn’t come from a PR firm.
I’ve seen patients crash after switching. Not statistically significant? Maybe. But I’ve seen it. With my own eyes.
And the refrigeration? Please. You think your CVS pharmacist knows how to handle a vial of biosimilar insulin? They’re just handing out flu shots and energy drinks.
This isn’t innovation. It’s cost-cutting dressed up as compassion.
Ben Harris
24/Dec/2025My cousin got switched to a biosimilar for her MS and now she’s got weird rashes and can’t walk right - they said it was ‘just stress’ but I know better. They’re testing us like lab rats and no one’s talking about it. You think they’d tell you if it was dangerous? Nah. They want you to stay quiet so they can keep raking in cash
Oluwatosin Ayodele
24/Dec/2025Actually, this is basic pharmacology. In Nigeria, we’ve been using biosimilars for over a decade because we can’t afford the originals. The WHO validates them. The data is solid. Your fear is not science - it’s privilege.
Also, generics don’t exist for biologics because you can’t replicate a living cell like you replicate a molecule. That’s not a flaw - it’s biology.
Stop pretending this is new. It’s just that rich countries are slow to catch up.
Jason Jasper
24/Dec/2025I’ve been on Humira for 8 years. My doc offered the biosimilar last year. I said yes. No side effects. No flare-ups. Just lower copay. Honestly? I’m glad I did. It’s not about the brand. It’s about staying healthy.
Carlos Narvaez
24/Dec/2025Let’s not confuse ‘similar’ with ‘identical.’ Biosimilars are not generics. That’s not a nuance - it’s a fundamental distinction. If you’re treating cancer or autoimmune disease, you need to understand that.
And yes - storage matters. I’ve seen a vial of insulin biosimilar ruined because it sat in a car for 4 hours. The patient didn’t know. That’s not the drug’s fault. It’s the system’s.
Harbans Singh
24/Dec/2025I’m from India - we’ve been using biosimilars for TNF inhibitors since 2014. My uncle got one for his Crohn’s. Saved him $15k/year. He’s still in remission. The science isn’t magic - it’s rigor. Don’t let fear silence progress.
Also - if your pharmacy doesn’t stock it, ask. Demand it. Change happens when people speak up.
Justin James
24/Dec/2025Here’s what they don’t tell you - biosimilars are the Trojan horse. First they swap your drug. Then they start changing the dosing. Then they cut your coverage. Then they drop the original entirely. It’s a slow burn. The FDA doesn’t care. Your doctor’s paid by the system. Your insurer? They’re laughing all the way to the bank. And you? You’re just the guinea pig who thinks they’re saving money. But what if the real cost is your life? What if the ‘no clinically meaningful difference’ is just a lie wrapped in jargon? I’ve seen people die after switching. They didn’t know. No one told them. And now the system says ‘it’s safe.’ But who’s counting the bodies?
Zabihullah Saleh
24/Dec/2025It’s funny how we fear what we don’t understand. We accept generics without blinking - because they’re pills. But when it’s a protein made by living cells? Suddenly it’s ‘too complex.’
But we eat genetically modified food, take vaccines made in chicken eggs, and trust robots to drive our cars. Yet a biosimilar? Too scary.
Maybe the real issue isn’t the drug. It’s our relationship with medicine - and how we’ve been taught to fear it.
Rick Kimberly
24/Dec/2025As a clinical pharmacist with 18 years of experience, I can confirm: biosimilars are held to the same regulatory standard as originators. The analytical comparability studies alone require over 100 parameters. The clinical trials are not ‘small’ - they are statistically powered and designed to detect even subtle differences.
Patients who report adverse events post-switch often have underlying anxiety or comorbidities - not drug failure.
It is not irresponsible to recommend biosimilars. It is ethical.
Terry Free
24/Dec/2025Oh wow, someone actually wrote a useful article? Shocking. You mean we don’t have to pay $20k for a drug that’s basically a protein soup? Who knew capitalism could be kind? Anyway, my insurance forced me to switch. I cried. Then I saved $5k. Now I’m buying a new bike. So… thanks, biosimilars. You’re not evil. Just expensive.
Sophie Stallkind
24/Dec/2025Thank you for this meticulously researched and clinically grounded exposition. The distinction between generics and biosimilars is not merely academic - it is a matter of patient safety, regulatory integrity, and equitable access. I commend the clarity with which this complex subject has been rendered accessible.