PINP: What It Is, Why It Matters, and How It Relates to Bone Health
When your body rebuilds bone, it doesn’t just randomly grow new tissue—it follows a precise process, and PINP, a protein fragment released when new bone is formed. Also known as procollagen type I N-terminal propeptide, it’s one of the most reliable ways to measure how fast your bones are making new material. Think of it like a factory output report: the more PINP in your blood, the more actively your bones are rebuilding themselves. This isn’t just academic—it’s used daily by doctors to track osteoporosis treatment, monitor healing after fractures, and even predict future bone loss.
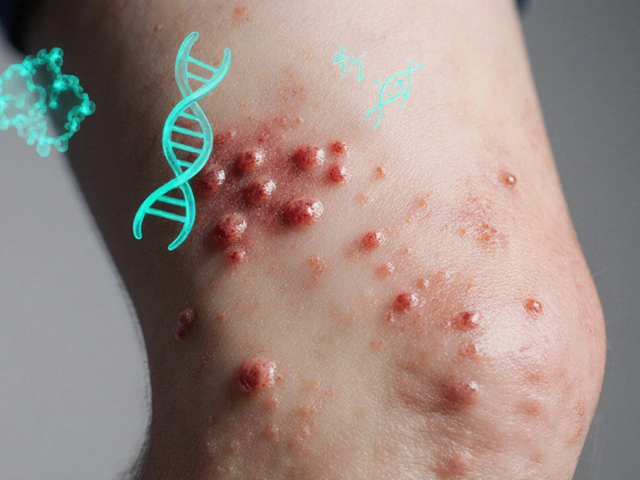
PINP doesn’t work alone. It’s part of a pair with bone resorption markers, substances released when old bone breaks down, like CTX or NTX. Together, they give a full picture: if PINP is high but resorption markers are higher, your bones are losing more than they’re gaining. If both are low, your bone turnover is sluggish—which can be just as risky. This balance matters most in people on drugs like bisphosphonates, medications that slow bone breakdown, or those recovering from long-term steroid use. Your PINP level can tell you if the treatment is working before a DEXA scan even shows a change.
It’s not just for seniors. PINP testing is increasingly used in younger adults with eating disorders, hormonal imbalances, or autoimmune conditions like rheumatoid arthritis—any situation where bone loss is a hidden risk. Athletes, especially women with low estrogen, often get checked too. Even if you’ve never had a fracture, a low PINP might mean your bones aren’t getting the renewal they need. And if you’re on a new osteoporosis drug, your doctor might check PINP after three months to see if it’s kicking in—faster than waiting a year for a scan.
The tests themselves are simple: a single blood draw, no fasting needed. But results need context. A high PINP doesn’t automatically mean you’re at risk—it could just mean you’re healing after surgery. A low level might reflect age, inactivity, or vitamin D deficiency. That’s why PINP is never read alone. It’s paired with your medical history, calcium levels, vitamin D status, and other bone markers. It’s a tool, not a diagnosis.
Below, you’ll find real-world stories and data-driven guides on how PINP fits into the bigger picture of bone health—from how it connects to medications like alendronate, to why some people see wild swings after starting treatment, to what happens when you stop osteoporosis drugs. These aren’t abstract studies. They’re practical insights from people who’ve been there, and the doctors who track PINP every day to keep bones strong.
Bone Turnover Markers: How They Help Monitor Osteoporosis Treatment
Bone turnover markers like PINP and β-CTX-I offer early, reliable insight into how well osteoporosis treatments are working-within weeks, not years. Learn how they guide therapy and improve outcomes.
Read