BPH Management: Effective Strategies to Relieve Prostate Symptoms
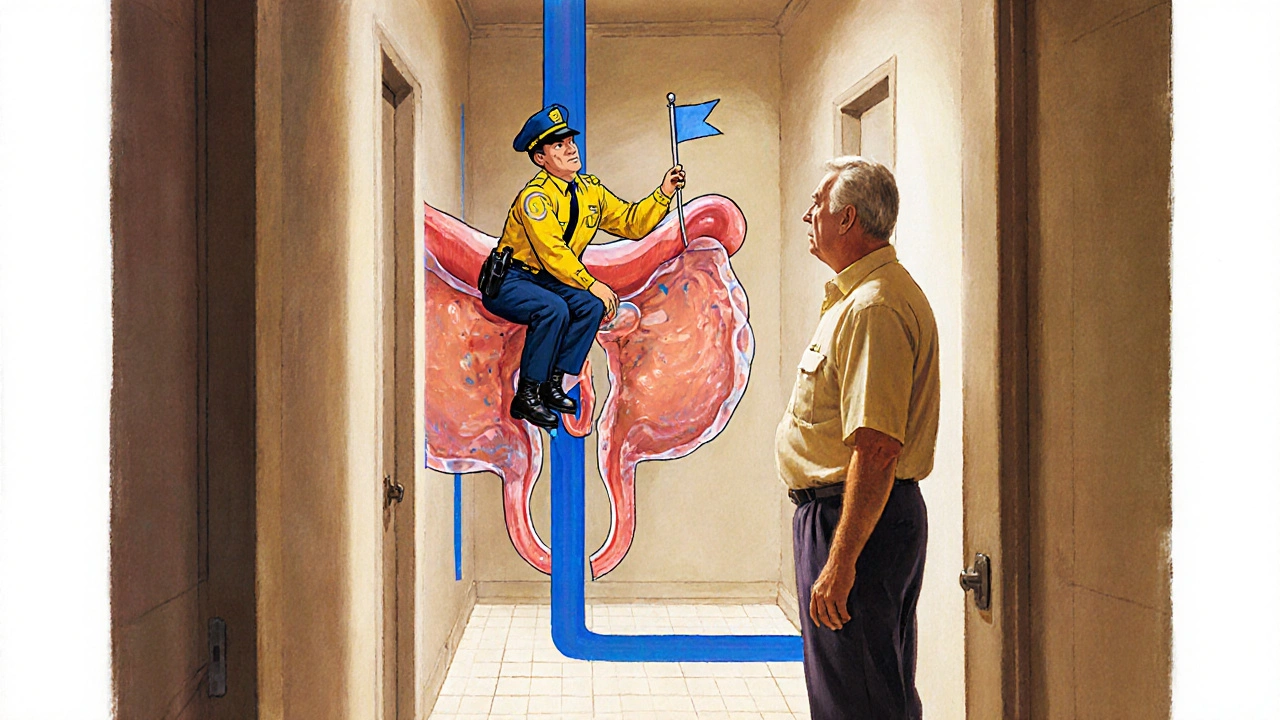
When dealing with BPH management, the set of approaches used to control benign prostatic hyperplasia, a non‑cancerous enlargement of the prostate gland that causes urinary problems. Also known as prostate enlargement treatment, it blends medication, lifestyle tweaks, and procedures to keep the flow smooth. This page pulls together the most useful info you’ll need to decide what works best for you, whether you’re just starting to notice symptoms or you’ve been handling them for years. Below you’ll see how each piece fits into the bigger picture of BPH management.
Key Pillars of BPH Management
One cornerstone is alpha blockers, drugs that relax the smooth muscle in the prostate and bladder neck to improve urine flow. They act fast, often easing symptoms within a week, and are a go‑to for men with moderate urgency. Another major class is 5‑alpha‑reductase inhibitors, medications that shrink the prostate over several months by blocking the hormone DHT. These are ideal when the gland is noticeably enlarged on ultrasound. Both drug groups can be used together, creating a synergistic effect that tackles muscle tension and gland size at the same time.
Beyond pills, lifestyle changes, dietary adjustments, fluid timing, and regular pelvic exercises that reduce pressure on the bladder play a surprisingly big role. Cutting back on caffeine and alcohol can calm nighttime trips, while a diet rich in tomatoes, broccoli, and omega‑3 fats may slow prostate growth. Simple habits like voiding on a schedule, avoiding large‑volume drinks before bedtime, and doing Kegel‑type exercises strengthen the pelvic floor and improve control. These tweaks don’t replace medication, but they often let you use lower doses and experience fewer side effects.
When symptoms persist despite meds and lifestyle tweaks, minimally invasive procedures, techniques such as UroLift, water‑vapor therapy, or transurethral resection that remove or compress prostate tissue without major surgery become options. They aim to keep the bladder emptying efficiently while preserving sexual function. In many cases, a single outpatient visit can deliver lasting relief, and recovery time is measured in days rather than weeks. Choosing the right procedure depends on prostate size, shape, and personal health, so a thorough discussion with a urologist is essential.
Monitoring is the glue that holds all these strategies together. Regular check‑ups let you track symptom scores, PSA levels, and prostate volume changes. If a medication stops working or side effects emerge, your doctor can adjust the regimen or suggest a procedure. Early detection of worsening blockage prevents complications like urinary retention or kidney damage. Keeping a simple diary of bathroom trips, flow strength, and nighttime awakenings gives your clinician concrete data to fine‑tune the plan.
Now that you have a clear picture of how medication, lifestyle, and procedures interlink, explore the articles below. You’ll find detailed comparisons of alpha blockers versus 5‑alpha‑reductase inhibitors, practical tips for diet and exercise, and step‑by‑step guides to the most common minimally invasive surgeries. Each piece is written to help you make informed choices and stay ahead of BPH symptoms.
Alfuzosin Guide: Safe & Effective BPH Treatment
A practical guide on using alfuzosin safely for benign prostatic hyperplasia, covering dosage, side effects, drug interactions, monitoring, and tips for optimal symptom relief.
Read