Tetanus Vaccination Impact Calculator
Enter values above to see impact statistics
When a community rolls out a tetanus vaccination program, it aims to protect people from a deadly bacterial infection that can enter through cuts or wounds, the results can be dramatic. Below you’ll find three standout examples, the tactics that made them work, and the pitfalls you’ll want to dodge when you design your own effort.
Why Tetanus Still Matters in 2025
Even though the tetanus vaccine has been around for decades, the disease kills an estimated 40,000 people each year, mostly in low‑resource settings. The World Health Organization (WHO) still lists tetanus among the top vaccine‑preventable threats for pregnant women and newborns. Recent data show that every $1 spent on a complete tetanus series can prevent up to 10 deaths, making it one of the most cost‑effective interventions available.
Success Story #1 - Thailand’s National Immunization Program
Thailand’s National Immunization Program (NIP) started in the early 1990s and now covers >95% of infants with the DTP vaccine. The program’s secret sauce?
- Strong political commitment: the health ministry earmarked a dedicated budget line for tetanus and other childhood vaccines.
- Integrated delivery: tetanus shots were given alongside measles and polio during outreach visits, reducing missed opportunities.
- Data‑driven micro‑planning: health officers used GIS maps to target remote villages and track coverage in real time.
By 2020, Thailand reduced neonatal tetanus cases from 2 per 1,000 live births to under 0.3, meeting the WHO elimination target a full decade ahead of schedule.
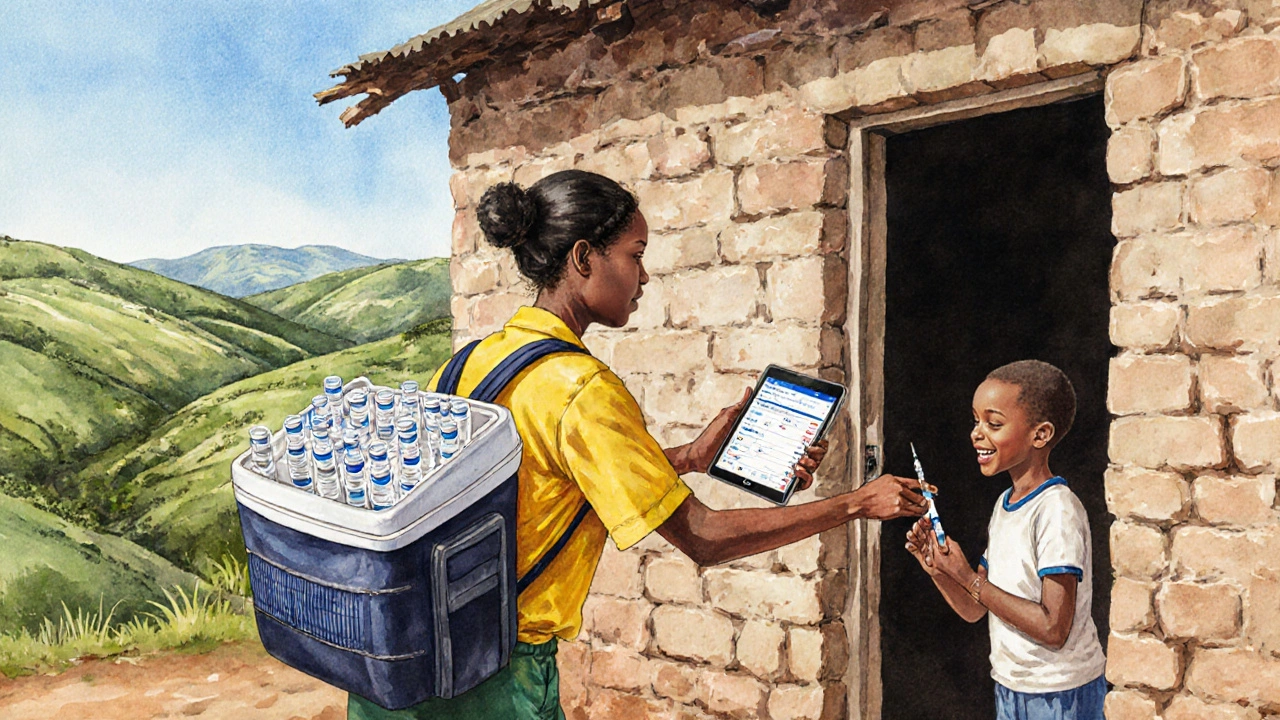
Success Story #2 - Rwanda’s Community Health Worker Model
Rwanda partnered with UNICEF to train a network of community health workers (CHWs) who deliver vaccines door‑to‑door in hard‑to‑reach areas. Key elements included:
- Performance‑based incentives for CHWs, tied to the number of fully immunized children they register.
- Mobile reporting tools that send daily coverage stats to district supervisors.
- Cold‑chain innovations, such as solar‑powered vaccine refrigerators, ensuring potency even in off‑grid villages.
Results speak for themselves: from 2015 to 2024, Rwanda’s tetanus coverage rose from 78% to 96%, and maternal tetanus deaths dropped by 85%.
Success Story #3 - Haiti’s Post‑Earthquake Campaign
After the 2021 earthquake, Haiti faced a surge in injuries and a fragile health system. The Ministry of Health, with support from the Global Vaccine Action Plan (GVAP) framework, launched an emergency tetanus vaccination drive targeting trauma patients and at‑risk communities. The approach combined:
- Rapid deployment of mobile clinics staffed by volunteer physicians.
- On‑site adverse event monitoring to reassure the public and maintain trust.
- Volunteer‑led education sessions that tackled vaccine myths head‑on.
Within six months, over 150,000 people received a tetanus booster, and the post‑disaster tetanus incidence fell to its lowest level in a decade.
Common Strategies That Powered Success
| Strategy | What it does | Typical impact |
|---|---|---|
| Political & financial commitment | Secures stable funding and policy backing | 10‑15% increase in coverage per year |
| Integrated service delivery | Combines tetanus with other routine shots | Reduces missed opportunities by ~30% |
| Community health worker engagement | Brings vaccines to doorsteps, especially in hard‑to‑reach areas | Boosts coverage in remote zones from 60% to >90% |
| Real‑time data & micro‑planning | Maps gaps, directs resources efficiently | Cut stockouts by 40% and improves target‑hit rates |
| Cold‑chain innovation | Maintains vaccine potency in off‑grid settings | Reduces wastage to <5% of doses |
| Adverse event monitoring & risk communication | Builds trust, mitigates hesitancy | Improves acceptance rates by up to 20% |
Lessons Learned - Pitfalls to Avoid
Every success story also revealed blind spots. Here are the top three mistakes that can derail a tetanus drive:
- Under‑estimating logistics. Even with solar fridges, transporting vaccines over rough terrain needs careful route planning. A miscalculation in the Philippines led to a 12‑hour delay and 8% dose loss.
- Ignoring cultural nuances. In some regions, women need husband approval before receiving vaccines. Programs that didn’t involve male community leaders saw lower uptake among expectant mothers.
- Failing to sustain funding. One East African pilot achieved 94% coverage, but after donor money dried up, coverage fell back to 68% within two years.
Address each of these early on, and you’ll keep momentum going long after the initial launch.

Actionable Checklist for New Tetanus Programs
- Secure a dedicated budget line from national or regional authorities.
- Map every health facility, mobile clinic site, and high‑risk community using GIS tools.
- Recruit and train community health workers; tie incentives to coverage metrics.
- Integrate tetanus shots with existing DTP, measles, or maternal health visits.
- Invest in solar‑powered cold‑chain equipment for off‑grid areas.
- Set up a rapid adverse‑event reporting system (SMS‑based works well).
- Develop culturally tailored communication materials; involve local leaders early.
- Establish a real‑time dashboard to monitor stock levels, coverage, and drop‑out rates.
Follow this list, and you’ll be on track to hit the WHO elimination threshold-less than 1 case per 1,000 live births-within five years.
Where to Find More Guidance
The World Health Organization offers a suite of technical manuals on tetanus elimination and supplemental immunization activities. Their latest 2024 “Tetanus Vaccine Deployment Toolkit” includes sample micro‑plans, budgeting templates, and monitoring checklists. Additionally, the UNICEF provides field‑tested training modules for community health workers, which you can adapt to local languages.
Frequently Asked Questions
What age groups should receive tetanus vaccination?
The standard schedule includes three doses for infants (usually combined as DTP), a booster at 12-15 months, and another booster during adolescence. Pregnant women should get a tetanus‑containing vaccine during each pregnancy if they haven’t received a dose in the previous three years.
How does cold‑chain failure affect vaccine efficacy?
Tetanus toxoid loses potency when exposed to temperatures above 8°C for prolonged periods. Studies show a 20% drop in immunogenicity after just 24hours in the “danger zone.” Maintaining the cold chain is therefore critical to ensure protective immunity.
Can tetanus be eliminated without eliminating all cases of wound infection?
Yes. The goal is to prevent toxin‑producing infections by ensuring everyone is immunized. Even if wounds become infected, a fully vaccinated person’s immune system neutralizes the toxin, averting severe disease.
What are the main reasons for vaccine hesitancy around tetanus?
Misinformation about safety, cultural beliefs that vaccines interfere with natural immunity, and lack of visible disease (since tetanus is rare where coverage is high) all fuel hesitancy. Tailored risk‑communication campaigns that involve trusted community figures are the most effective counter‑measures.
How long does protection from a tetanus booster last?
A single booster provides protection for about 10 years. After that, a repeat dose is recommended, especially for individuals with high exposure risk (e.g., agricultural workers, soldiers).






Comments
Keli Richards
12/Oct/2025Interesting data on how a $1 spend can save lives
Ravikumar Padala
12/Oct/2025The article does a decent job of outlining the major programs, but it could use more depth on the financing mechanisms. Thailand’s budget allocation, for instance, was not just a line item but part of a broader health reform agenda that spanned decades. The integration of tetanus with measles and polio shots reduced logistical overhead, yet the piece barely mentions cold‑chain constraints in remote villages. Rwanda’s community health worker incentives were tied to exact numbers of fully immunized children, which created a data‑driven culture, and that nuance is worth highlighting. The mobile reporting tools they used were based on open‑source platforms that allowed local technicians to customize dashboards, a detail that resonates with tech‑savvy planners. Haiti’s post‑earthquake response also leveraged volunteer physicians, but the coordination between NGOs and the Ministry of Health required a rapid legal framework that the article glosses over. Moreover, the cost‑effectiveness metric of ten lives per dollar, while striking, depends heavily on local health system efficiency, something the author could elaborate on. The use of GIS micro‑planning in Thailand is a model that other nations could replicate, but the article doesn’t discuss the training required for health officers to interpret those maps. The solar‑powered refrigerators in Rwanda mitigate power outages, yet their maintenance schedules and funding sources are rarely mentioned. The piece also skips over the challenges of vaccine hesitancy, which remain a barrier even in high‑coverage areas. While the table of strategies is useful, it could benefit from real‑world anecdotes that illustrate each point. The narrative would be stronger if it addressed the political risks when governments shift priorities mid‑term. Overall, the article provides a solid foundation but leaves many implementation details for the reader to infer, which limits its practical utility for program designers.
King Shayne I
12/Oct/2025This so‑called ‘success story’ is just fluff, ignore the hype.
jennifer jackson
12/Oct/2025Glad you pointed that out! Keep the good vibes
Brenda Martinez
12/Oct/2025Honestly, the whole “real‑world success” narrative feels like a staged PR stunt. They cherry‑pick Thailand, Rwanda, and Haiti, ignoring countless failures that never make the headlines. The drama of dropping neonatal tetanus rates is presented as if it happened overnight, when in reality it required decades of relentless funding, political will, and frankly, a lot of trial and error. If you’re looking for a balanced view, ask yourself why the article never mentions the massive stock‑outs that plagued Rwanda’s cold‑chain before solar fridges arrived. It’s a classic case of selective storytelling, and readers deserve the full picture, not just the glossy highlights.
Marlene Schanz
12/Oct/2025Actually, the successes aren’t as rare as they seem. Thailand’s health ministry set aside a dedicated budget line for vaccines back in the ’90s, which helped steady the cash flow. The GIS maps they used were open‑source, so local NGOs could adapt them without paying big licences. Also, Rwanda’s CHWs got performance bonuses based on the number of kids fully immunized – that incentive system drove a lot of the coverage jump. Hope that adds some practical insight.
Matthew Ulvik
12/Oct/2025Great rundown! 👍 The integration tip is super useful – bundling tetanus with other shots really cuts down on missed appointments. If anyone’s building a program, start by mapping out where you can piggyback on existing outreach.
Dharmendra Singh
12/Oct/2025Thanks for the practical note. In India we’ve seen similar success when we combine tetanus with the polio drives, especially in hard‑to‑reach villages. The key is reliable cold‑chain, even if you have to use portable ice packs.
Rocco Abel
12/Oct/2025While the article is informative, one must consider the underlying socioeconomic disparities that drive vaccine uptake. The elite perspective often overlooks grassroots empowerment, which is the true catalyst for sustainable health outcomes.
Dawn Mich
12/Oct/2025Don’t get lost in lofty theories – the real issue is that big‑pharma pushes these numbers to keep funding flowing, regardless of whether the on‑the‑ground reality matches the stats. People deserve transparency, not polished propaganda.