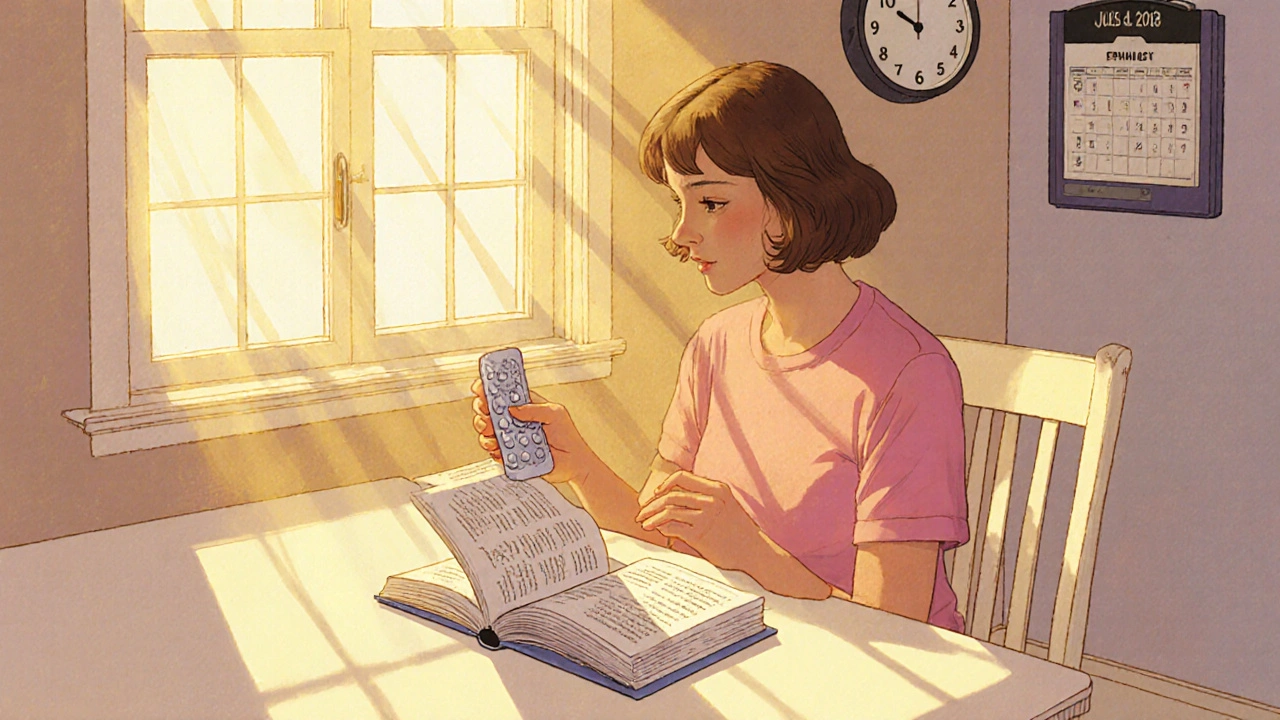
Progesterone-Only Pill – Everything You Need to Know
When working with progesterone-only pill, a daily oral contraceptive that relies solely on synthetic progestin to prevent pregnancy. Also known as mini‑pill, it offers an estrogen‑free option for many users. It belongs to the broader category of hormonal contraception, which includes methods that use hormones to block ovulation or create an inhospitable uterine environment. The active ingredient, progestin, mimics natural progesterone and binds to progesterone receptors in the body. By altering the menstrual cycle, the pill thins the uterine lining and stiffens cervical mucus, making sperm entry difficult.
How It Works and Who Might Choose It
The mini‑pill works through three linked actions, a classic semantic triple: progesterone‑only pill → prevents ovulation → creates thick cervical mucus. In most cycles it stops the egg from being released, but even when ovulation occurs the thick mucus acts as a barrier. At the same time, the progestin‑driven thinning of the endometrium reduces the chance of implantation. Because there’s no estrogen, the pill avoids estrogen‑related risks like blood clots, making it a go‑to choice for breastfeeding moms, women over 35 who smoke, or anyone with estrogen sensitivity.
Another triple ties side effects to hormone action: progestin → changes in bleeding pattern → spotting or lighter periods. Users often notice irregular spotting during the first months, then many report lighter, more predictable periods once the body adapts. Some experience acne improvement because progestin can counteract androgen‑driven skin issues. On the flip side, a minority feel mood swings or breast tenderness—effects linked directly to how progestin interacts with brain receptors.
Choosing the mini‑pill also depends on lifestyle. It requires strict timing—take it at the same hour each day—because a delay of more than three hours can reduce effectiveness. For people who struggle with daily schedules, a longer‑acting method like an IUD might be better. However, the pill’s fast return to fertility after stopping is a big selling point for those planning pregnancy soon.
Understanding drug interactions is key. Certain antibiotics, anticonvulsants, and herbal supplements (like St John’s wort) can lower progestin levels, potentially weakening protection. Always check with a pharmacist or doctor before adding new meds. This knowledge connects the entities of drug interactions and contraceptive efficacy, another semantic link that guides safe use.
From a health‑economics view, the mini‑pill is inexpensive and widely covered by insurance, a fact that influences its popularity across different income groups. Its low cost, combined with the absence of estrogen‑related monitoring, keeps long‑term expenses down—a practical consideration for anyone budgeting their healthcare.
For those curious about switching from combined pills, the transition is simple: stop the combined pill and start the mini‑pill the same day. No wash‑out period is needed, but a backup method (like condoms) should be used for the first 48 hours while the body adjusts. This step‑by‑step shift highlights the relationship between combined oral contraceptives and progesterone-only pills, showing how one can move within the hormonal contraception family.
When it comes to side‑effect management, lifestyle tweaks help. A balanced diet rich in calcium and vitamin D supports bone health, which can be slightly impacted by low estrogen levels. Regular exercise and stress‑reduction techniques (like yoga or breathing exercises) may ease mood changes. If heavy spotting persists beyond three months, a quick visit to a healthcare provider can rule out underlying issues.
Finally, remember that the mini‑pill does not protect against sexually transmitted infections (STIs). Pairing it with condoms offers both pregnancy prevention and STI protection—a dual benefit that aligns with public‑health recommendations.
Below you’ll find a curated set of articles that dive deeper into each of these points, from detailed side‑effect profiles to real‑world user experiences. Explore the collection to get the practical answers you need for confident contraceptive choices.
Desogestrel and Fertility: Essential Guide for Trying to Conceive
Learn how desogestrel affects fertility, when ovulation returns after stopping, and practical tips for women trying to conceive.
Read