Azathioprine is a drug many people take to stop their immune system from attacking their own body. It’s used for autoimmune diseases like rheumatoid arthritis, Crohn’s disease, and after organ transplants. But for some, it doesn’t just calm the immune system-it starts breaking down muscle. That’s called drug-induced myopathy. It’s not rare. It’s not always noticed. And if you’re on azathioprine and feel your legs getting weaker, or you can’t climb stairs like you used to, you need to know what’s happening.
What Azathioprine Does in Your Body
Azathioprine is a prodrug. That means your body turns it into another chemical-6-mercaptopurine (6-MP)-before it starts working. That active form blocks DNA and RNA production in fast-dividing cells, especially immune cells. Less immune activity means less inflammation. That’s good for someone with lupus or a transplanted kidney. But muscle cells aren’t supposed to be the target. Yet sometimes, they are.
Why? Because muscle cells, especially under stress or with genetic risk factors, can accidentally absorb and process azathioprine the same way immune cells do. The drug interferes with mitochondrial function-the energy factories inside your muscle cells. Without enough energy, muscles can’t contract properly. They start to waste away. This isn’t just fatigue. It’s actual muscle loss.
What Drug-Induced Myopathy Feels Like
If you’ve been on azathioprine for months or years and suddenly notice you’re getting weaker, don’t brush it off as aging. Drug-induced myopathy doesn’t come with swelling or pain. It’s quiet. You might think you’re just out of shape. But here’s what it actually looks like:
- Struggling to stand up from a chair without using your arms
- Needing to hold onto railings when going up stairs
- Falling more often, even on flat ground
- Difficulty lifting grocery bags or opening jars
- Muscles feeling ‘heavy’ or ‘dead’ even after rest
These symptoms usually show up slowly. Over weeks or months. Often, doctors blame it on inactivity, arthritis, or vitamin D deficiency. But if you’re on azathioprine and these signs appear, it’s time to check for myopathy.
Who’s Most at Risk
Not everyone on azathioprine gets muscle damage. But some people are far more likely to. Risk factors include:
- Being over 65
- Having kidney problems (azathioprine is cleared by the kidneys)
- Taking it with other drugs like statins or colchicine
- Having a genetic variation in the TPMT gene
The TPMT gene controls how your body breaks down azathioprine. About 1 in 300 people have a version of this gene that makes them process the drug extremely slowly. That means the drug builds up in their blood. Higher levels = higher risk of muscle damage. Genetic testing for TPMT is standard before starting azathioprine in many hospitals-but not all. If you haven’t had this test, ask your doctor if it’s been done.
Also, combining azathioprine with statins (like atorvastatin or simvastatin) is a red flag. Both drugs can hurt muscle tissue. Together, they multiply the risk. If you’re on both, your muscle weakness could be coming from the combo-not just one of them.
How Doctors Diagnose It
If your doctor suspects azathioprine-related myopathy, they won’t just guess. They’ll look for clear signs:
- Blood test: Elevated creatine kinase (CK) levels. CK is a protein that leaks out of damaged muscle. Normal is under 200 U/L. Levels over 1,000 U/L are a strong signal.
- Electromyography (EMG): A small needle is inserted into your muscle to check electrical activity. In drug-induced myopathy, you’ll see abnormal patterns-like low-amplitude signals or early recruitment.
- Muscle biopsy: The gold standard. A tiny piece of muscle (usually from the thigh) is taken and looked at under a microscope. You’ll see damaged mitochondria, fat buildup, and fiber breakdown. It’s invasive, but it’s the only way to be 100% sure.
- Response to stopping the drug: If your weakness improves within weeks after stopping azathioprine, that’s a major clue.
Some doctors skip the biopsy and go straight to stopping the drug. That’s acceptable if the symptoms are clear and CK is high. But if the cause is unclear, a biopsy rules out other diseases like polymyositis or ALS.
What Happens When You Stop Azathioprine
Stopping azathioprine doesn’t mean your autoimmune disease comes roaring back overnight. For many, symptoms improve slowly. Muscle strength often starts coming back in 4 to 8 weeks. Full recovery can take 3 to 6 months. But it’s not guaranteed. If muscle damage was severe or went on too long, some weakness may stay.
Doctors usually switch you to another immunosuppressant. Common alternatives include:
- Mycophenolate mofetil - Less muscle toxicity, widely used in transplant patients
- Cyclosporine - Effective but carries kidney and blood pressure risks
- Low-dose methotrexate - Often used for rheumatoid arthritis
None of these are risk-free. But none cause myopathy as often as azathioprine. Your doctor will pick based on your condition, kidney function, and other meds you take.
How to Prevent It
Prevention starts before you even take the first pill.
- Get tested for TPMT gene status before starting azathioprine. If you’re a slow metabolizer, your dose should be cut by 70-90%. Some people can’t take it at all.
- Avoid combining azathioprine with statins unless absolutely necessary. If you need both, use pravastatin or rosuvastatin-they’re less likely to harm muscle tissue.
- Get your CK levels checked every 3 months during the first year, then every 6 months after that. If CK doubles from baseline, get evaluated.
- Report any new weakness, even if it’s mild. Don’t wait until you can’t walk.
- Stay active. Light resistance training helps maintain muscle mass. Don’t become sedentary because you’re scared.
There’s no magic supplement or vitamin that prevents azathioprine myopathy. Coenzyme Q10? Creatine? Studies show no clear benefit. The only proven protection is careful monitoring and early action.

What to Do If You’re Already Affected
If you’ve been diagnosed with drug-induced myopathy from azathioprine:
- Don’t stop the drug on your own. Work with your doctor. Abruptly stopping can trigger a flare of your autoimmune disease.
- Ask for a referral to a neurologist or rheumatologist who’s seen this before. Not all doctors know how to manage it.
- Start physical therapy. A therapist can design a safe program to rebuild strength without overloading damaged muscles.
- Monitor your progress. Keep a simple log: how many stairs you can climb, how long it takes to get out of a chair. Small improvements matter.
- Ask about switching to mycophenolate. It’s now the first-line alternative in many guidelines for patients who develop myopathy.
Recovery isn’t linear. Some days you’ll feel better. Others, you’ll feel stuck. That’s normal. Muscle rebuilds slowly. Patience and consistency are your allies.
When to Seek Emergency Help
Most cases of azathioprine myopathy are slow and manageable. But if you suddenly develop:
- Severe muscle pain or swelling
- Dark urine (like cola)
- Difficulty breathing
- High fever with weakness
-go to the emergency room. These could mean rhabdomyolysis, a life-threatening condition where muscle breaks down so badly it floods your kidneys with toxins. It’s rare with azathioprine alone, but possible if you’re dehydrated, taking other drugs, or have kidney disease.
Final Thoughts
Azathioprine saves lives. But it’s not harmless. Drug-induced myopathy is underdiagnosed because it’s slow, painless, and easy to mistake for aging or inactivity. If you’re on this drug and feel weaker than you should, speak up. Push for a CK test. Ask about your TPMT status. Don’t let silence cost you your mobility.
There’s no shame in needing to switch medications. Your body’s health matters more than sticking with a drug just because it’s been prescribed for years. The goal isn’t just to survive your disease-it’s to live well while you do.
Can azathioprine cause permanent muscle damage?
Yes, if muscle damage is left untreated for months or years, some weakness can become permanent. Early detection and stopping the drug significantly improve recovery chances. Most people regain strength within 3-6 months after switching medications, but severe cases may leave lasting deficits.
Is muscle weakness from azathioprine reversible?
In most cases, yes. Muscle strength typically begins improving within 4-8 weeks after stopping azathioprine. Full recovery can take up to 6 months. Physical therapy and staying active during recovery greatly improve outcomes.
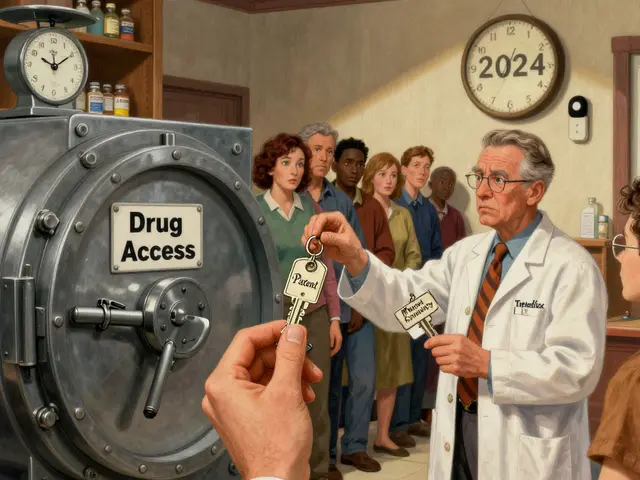
Should I get tested for TPMT before taking azathioprine?
Absolutely. The TPMT gene test is recommended by major medical guidelines before starting azathioprine. It identifies people who metabolize the drug slowly and are at high risk of toxicity-including muscle damage. If you haven’t had this test, ask your doctor for it.
Can I take statins while on azathioprine?
It’s risky. Combining azathioprine with statins increases the chance of muscle damage. If you need cholesterol medication, ask your doctor about pravastatin or rosuvastatin-they’re less likely to interact. Avoid simvastatin and atorvastatin if possible.
What’s the best alternative to azathioprine if I develop myopathy?
Mycophenolate mofetil is the most common and safest alternative. It’s effective for autoimmune diseases and transplant patients, with much lower risk of muscle toxicity. Cyclosporine and methotrexate are other options, but they have different side effect profiles. Your doctor will choose based on your condition and overall health.





Comments
Zac Gray
18/Nov/2025Let’s be real-this post reads like a pharmaceutical pamphlet written by a grad student who just discovered mitochondria. Azathioprine doesn’t ‘accidentally’ target muscle cells. It’s a blunt instrument. And yes, your body turns it into 6-MP, but that’s like saying a chainsaw ‘accidentally’ cuts your foot off when you’re trimming hedges. You knew the risks. You just didn’t want to hear them. And now you’re surprised your quads feel like wet newspaper? Shocking. Get your TPMT tested before you start another drug that turns your body into a chemical experiment. And stop blaming aging. You’re 42, not 82.
Ellen Calnan
18/Nov/2025I’ve been on azathioprine for 7 years. I thought my weakness was just ‘getting older’-until I couldn’t lift my dog into the car. No pain. No swelling. Just… dead legs. I cried in the vet’s office. Not because of the dog. Because I felt like a burden to my own body. This post? It’s the first time someone put words to what I’ve been feeling silently for years. Thank you. I got my CK checked last week-1,400. Stopped the drug. Switched to mycophenolate. Physical therapy started Monday. I’m not fixed. But I’m finally seen.
Brian Rono
18/Nov/2025Wow. Someone actually wrote a comprehensive, accurate, non-sensationalized piece about drug-induced myopathy. I’m stunned. Most ‘health influencers’ just scream ‘STOP ALL DRUGS!’ or ‘TRUST YOUR DOCTOR!’ This? This is medicine as it should be communicated: evidence, nuance, clarity. The TPMT gene point? Crucial. The statin combo warning? Lifesaving. The muscle biopsy detail? Perfect. This should be required reading for every rheumatology resident. And for patients? It’s the antidote to TikTok misinformation.
Richard Risemberg
18/Nov/2025Ellen’s comment hit me right in the chest. I’ve been a physical therapist for 18 years. I’ve seen dozens of patients with this exact slow-motion muscle collapse-always misdiagnosed as ‘deconditioning.’ One guy thought he was just lazy until he couldn’t get off the toilet without a grab bar. We started him on resistance bands, mobility drills, and a referral to his rheumatologist. He stopped azathioprine. Two months later, he walked his daughter down the aisle at her wedding. No cane. No help. Just him. That’s the power of early recognition. Don’t wait for the ‘cola-colored urine’ to act. If your legs feel like lead weights after a nap? That’s not fatigue. That’s your mitochondria screaming.
James Ó Nuanáin
18/Nov/2025As a British medical historian, I must say this is an exemplary piece of clinical communication. The structure, the precision, the avoidance of alarmism-truly commendable. That said, I must correct one minor point: the reference to ‘6-mercaptopurine’ as the active metabolite is technically accurate, but in pre-1980s literature, it was often referred to as ‘6-MP’ without the hyphen. A small orthographic quibble, but one that matters in archival accuracy. Also, I must note that the TPMT gene was first identified in 1981 by Dr. L. A. Weinshilboum at the Mayo Clinic. A footnote for the curious. And yes-pravastatin over simvastatin. Always. The pharmacokinetics are simply superior.
seamus moginie
18/Nov/2025Finally. Someone who doesn’t just say ‘take CoQ10’ and call it a day. I’ve been screaming into the void for years that this isn’t about supplements-it’s about monitoring. My uncle died from rhabdo because his doctor ignored his CK levels. He was on azathioprine AND simvastatin. They told him ‘it’s just muscle soreness.’ He was 58. Don’t be him. Get tested. Get checked. And if your doctor brushes you off? Find a new one. Your legs aren’t optional.
Michael Petesch
18/Nov/2025As someone who grew up in a household where ‘doctor knows best’ was gospel, this post changed my perspective. I’m 67, on azathioprine for Crohn’s since 2012. I thought my reduced stamina was just age. Turns out, my CK was 980. I didn’t know what CK was. I didn’t know about TPMT. I didn’t know statins could make it worse. I’m switching to mycophenolate next week. I’m not angry. I’m just… grateful someone wrote this in plain language. Thank you. I’m sharing this with my entire book club.
Steve and Charlie Maidment
18/Nov/2025So… you’re saying if I feel weak, I should stop the drug? What if I relapse? What if I die from my disease? This post is basically telling people to gamble with their lives. I’ve been on this for 10 years. I’m fine. Why are you scaring people? Maybe you just need to exercise more. Or take vitamin D. Or stop being lazy. Everyone’s so quick to blame the drug. Maybe your body’s just broken.